95% of surveyed doctors do not feel Australian PPE guidelines are accurate or up-to-date.
Such guidelines have unintended negative consequences including a great deal of uncertainty, shaming, bullying and harassment as well as rigid top down thinking in the workforce around this issue.
This in turn leads to the gravest forms of Post Traumatic Stress.
A letter (with great thanks) from Dr Karen Williams, Consultant Psychiatrist:
As a psychiatrist I am concerned about the vulnerability of my colleagues to PTSD. My experiences of speaking to a number of these doctors over the previous weeks have led me to contact you to request we raise the issue of the impact of current PPE guidelines on the workforce.
In order to ensure that the basis of my concerns had validity I posted an anonymous survey in a variety of online Australian medical forums. The response was extraordinarily rapid with 245 doctors replying in less than 24 hours. Approximately 65% of the respondents work in the hospital setting.
Preliminary Results
Whilst the survey continues the results so far have been marked.
- Less than half of the doctors had access to N95/P2 when required
- 23% of the doctors did not have access to surgical masks when required
- 6% of the doctors reused the same mask between patients
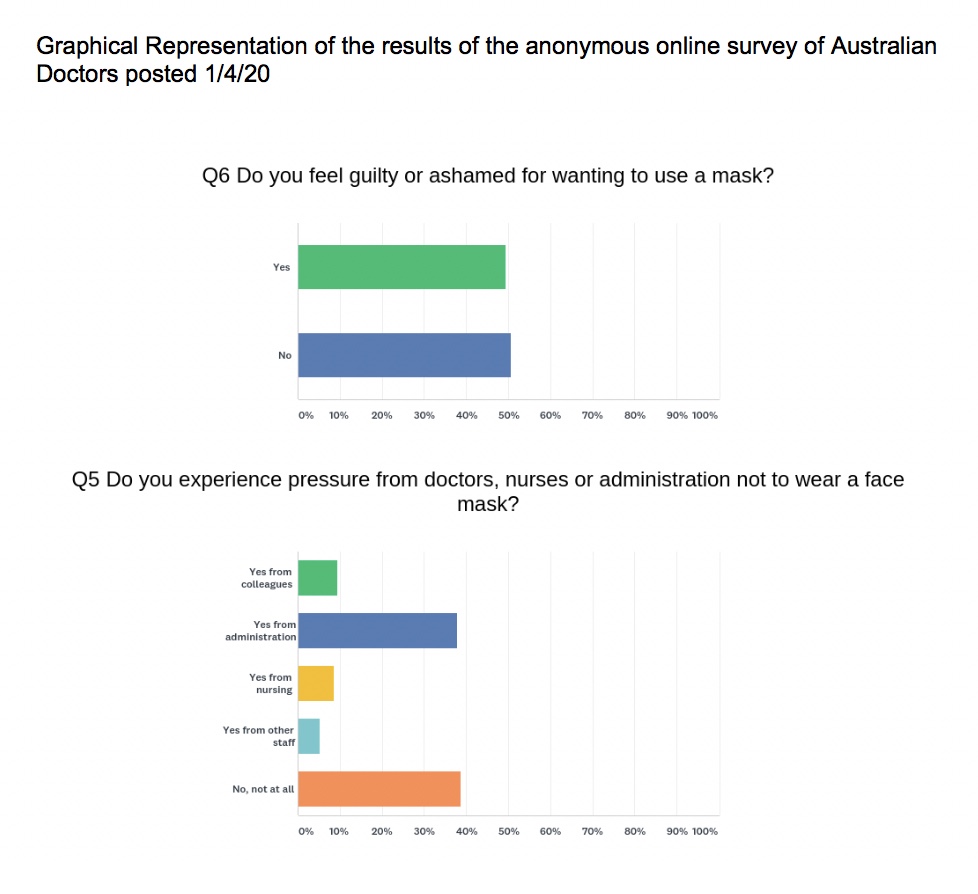
- 61% of doctors felt pressure from other staff not to wear a mask
- More than half of the doctors felt guilt/shame for wearing a mask
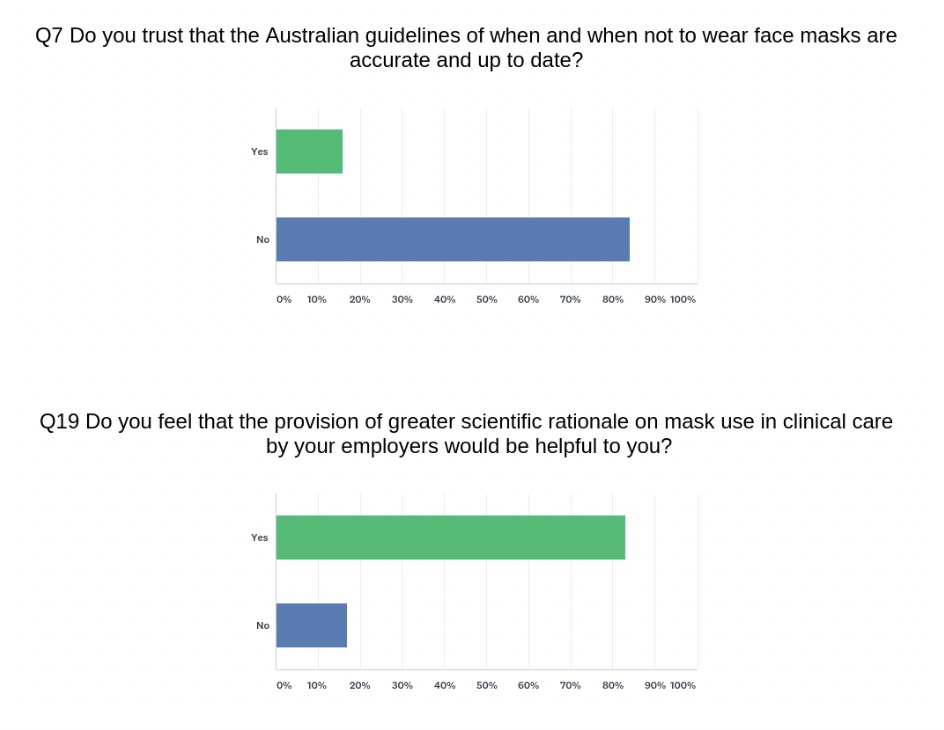
- 95% of the doctors surveyed (n= 204) did NOT trust that the Australian guidelines were accurate or up-to-date
- 86% of the doctors surveyed felt anxious about the level of PPE provided to them during the pandemic
- At least 80 respondents had been asked NOT to wear their own PPE to work
- 14 doctors said they would still see a patient with a confirmed diagnosis of COVID19 even if they had no mask
- 75% of doctors did not think Australian guidelines on mask usage were clear
- 85% of doctors did not think Australian guidelines on mask usage were consistent
- 56 doctors said that their supervisors were unwilling to speak to them about their concerns
- 50 doctors felt that their employment was threatened because of voicing concerns on face masks
- At least 55 doctors described being unable to speak out truthfully because of fears of reprisals
- 8% of doctors experienced bullying and harassment because of their views on masks
- 83% of doctors felt that provision of greater scientific rationale for mask use policy by employers would be helpful to them
Other comments from the survey:
Whilst there is an understanding of the shortage of masks at this time, the lack of a consensus of a truly gold standard use of PPE for all doctors, regardless of specialty, is causing considerable ‘dissent’ amongst doctors. Combined with a wide-spread concern that the current recommendations may be compromised by a fear that the hospitals will ‘run out’ before the crisis really peaks.
There is concern that there is a lack of normal scientific rigour in the development of guidelines on an intervention that is relatively cheap, simple and effective for reducing most large droplet and aerosol transmission and that this is causing our hospital doctors to be put directly at risk.
The main issues regarding the veracity of departmental guidelines include:
- Observations of the rates of infection in Asian countries who have been able to ‘flatten the curve’ and the fact that these countries have instituted greater barrier methods for health care workers
- An over representation of health care workers amongst COVID positive patients
- A growing body of evidence that transmission may not be as simple as droplet spread – with evidence of airborne transmission described in a variety of journals
- The limitation on evidence that we do NOT have community spread at this time which continues to factor in to the accessibility of screening
- The lack of acknowledgement of the issue of asymptomatic carriers in the guidelines.
- A number of papers including systematic reviews that mask use DOES reduce viral transmission and or aerosol droplet spread.
Conclusions
In my clinical opinion, based on the discussions I have had with doctors in person, on the phone and online , as well as the actual real threat of death or serious illness , our doctors are at real risk of traumatic syndromes such as PTSD.
I do understand that some things are not in our control, however strongly believe we can reduce the risk and impact of this situation on doctors mental health and improve the longevity of the workforce if we address this particular issue promptly and comprehensively.
I am aware that there is a collection of scientific papers including a systematic review on mask use during the SARS outbreak that shows a significant benefit of mask use. I am not aware of any systematic review that conclusively demonstrates that masks do not reduce viral transmission and risk for frontline workers, however if this was available and could be made available to doctors this would certainly alleviate their concerns. The fact that 83% of doctors surveyed did in fact answer that scientific literature would be useful to them demonstrates this.
I believe that the current Australian guidelines, whilst intended to acknowledge the supply issues have had unintended negative consequences including a great deal of uncertainty, shaming, bullying and harassment as well as rigid -thinking in the workforce around this issue. This is directly resulting in numerous instances of unsafe clinical practice.
If homemade masks for all staff is better than nothing then this should be clearly elucidated.
My concerns are as a human being first, and as a psychiatrist who works mainly with Post Traumatic Stress Disorder. I am a concerned citizen who can see many parallels to what is happening on the frontline for our doctors, to the stressors amongst military personnel that often result in poor prognosis.
Yours Sincerely
Dr. Karen Williams
Consultant Psychiatrist
Graphical Representation of the results of the anonymous online survey of Australian Doctors posted 1/4/20: