
Groupthink: A cultural phenomenon where group-self-reflection is discouraged to preserve group identity and unity.
A mythical experiment is often used to illustrate groupthink – 5 hungry monkeys in a cage attack any monkey in the cage who tries to grab a banana – an experimental punishment dished out to the whole group when the bananas are touched.
The video below shows a modern twist on this experiment – a patient in a waiting room is influenced to stand up on hearing a beep because others are doing it. She then perpetuates this phenomenon to others.
Overcoming groupthink is extremely difficult and can take an embarrassingly long time – particularly in an authoritative top down command structure.
Practices maintained through command structures often go unchallenged through fear. They can be perpetuated and reinforced for years – read an amusing example here – signing a bicycle register at one hospital for those who rode to work. The register originated in the days of rationing during WWII and was of no relevance for the next 60 years – however it persisted.
Perhaps the #TheatreCapChallenge demonstrates the sheer grip of groupthink and social conformity. Within a command structure staff feel threatened doing anything which is not dictated from the top down. These threats aren’t only imagined – they’re real. We all have mouths to feed and most of us have mortgages to pay – are we going to risk it?
In most instances it appears not – a real shame given we work in a high risk industry – in not changing we won’t improve and patients lives are left at unnecessary risk.
Failure to adopt the #TheatreCapChallenge perhaps illustrates the negative grip of groupthink in healthcare.
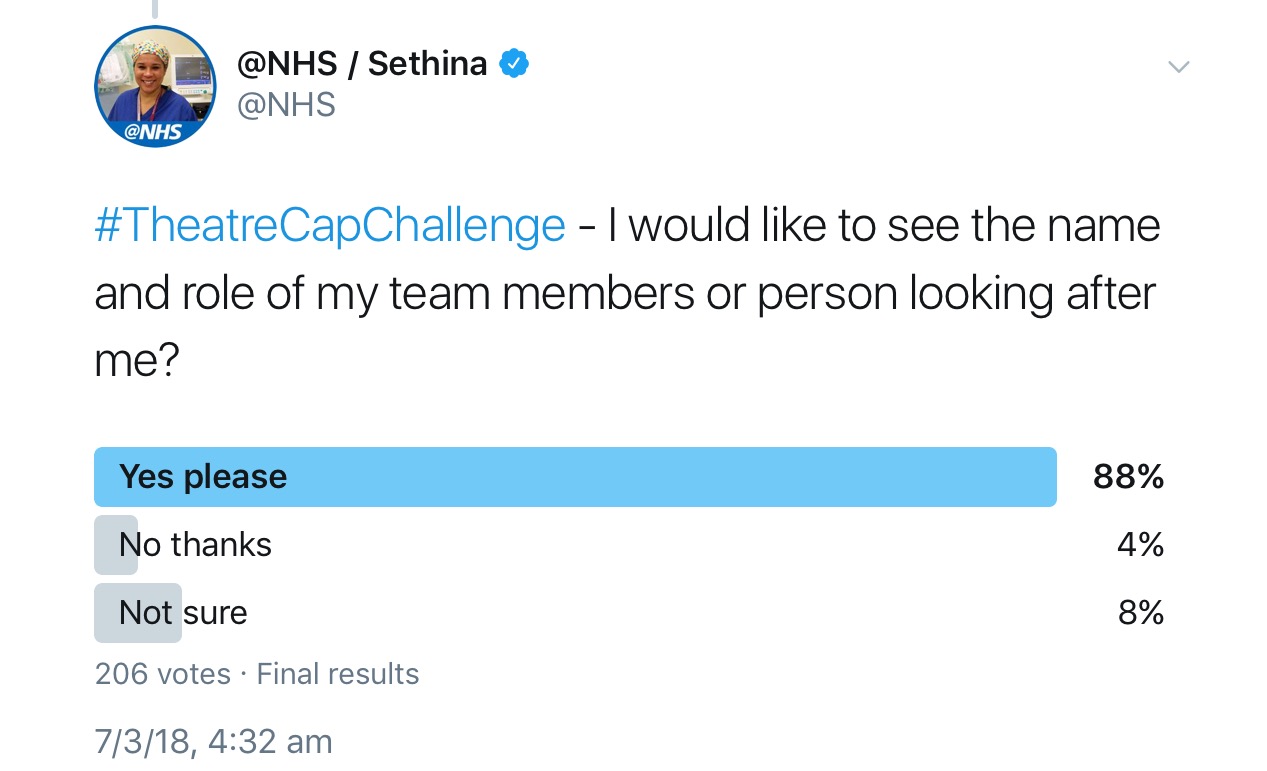
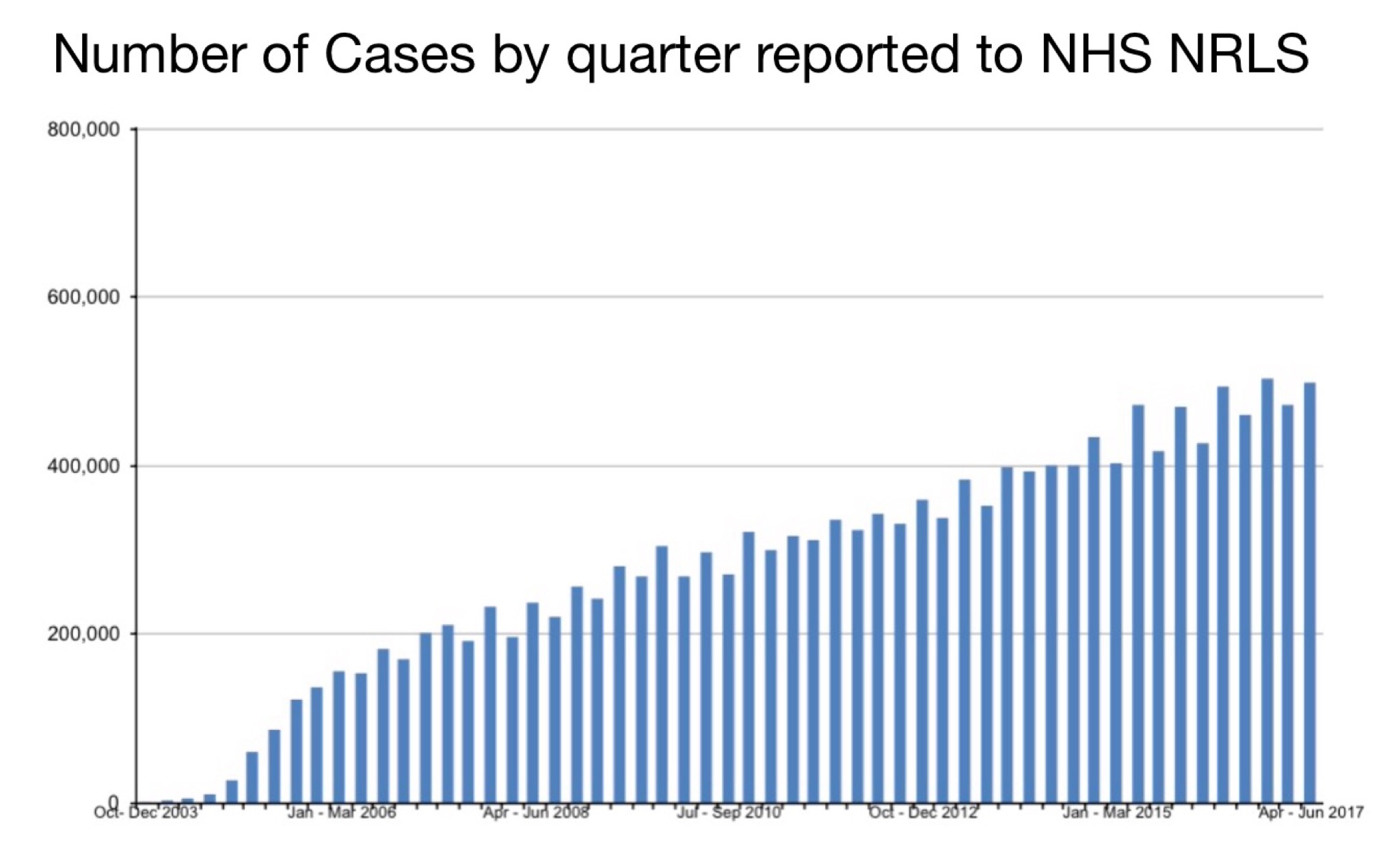
The initiative has overwhelming support from patients
and front line staff alike:
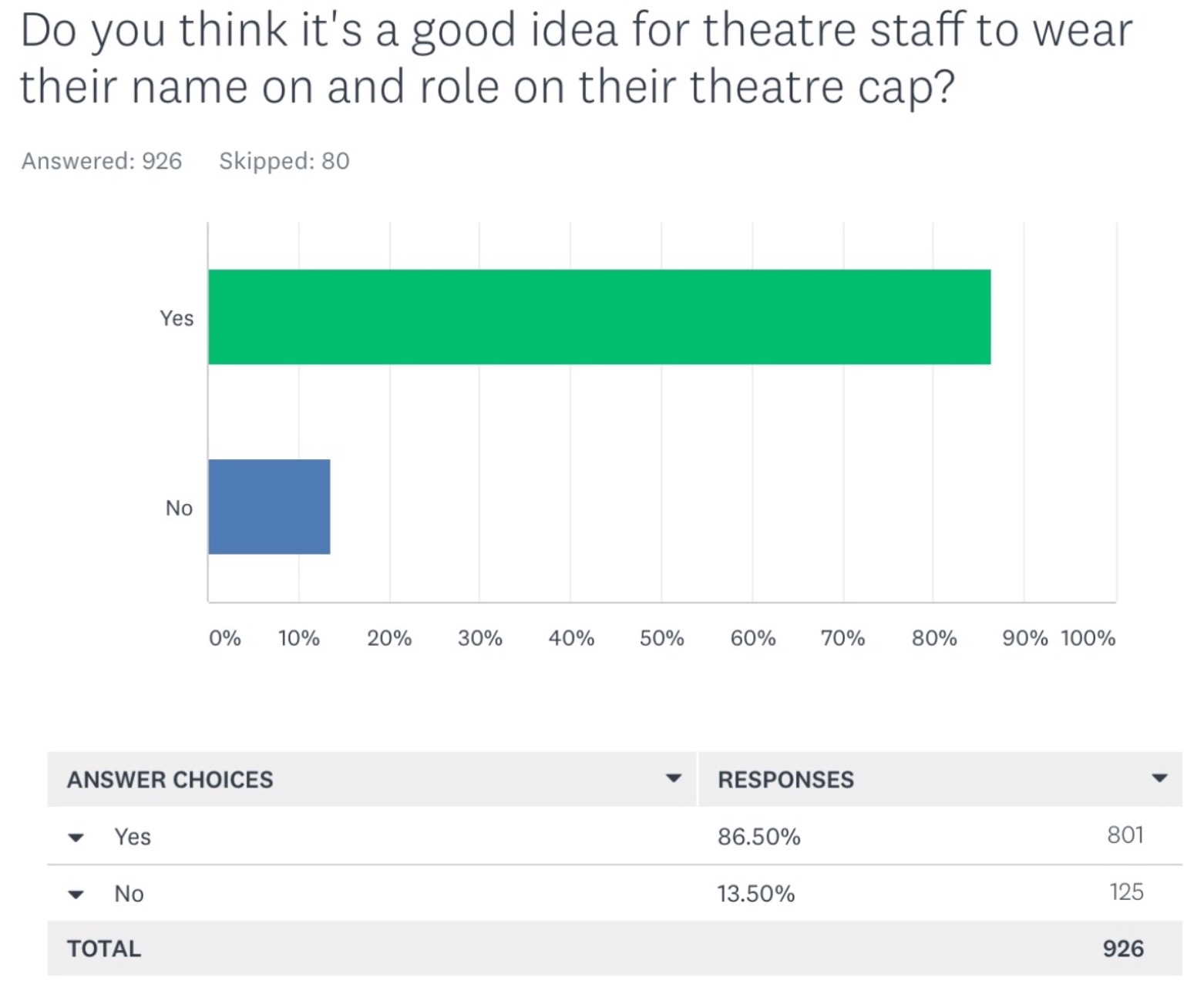
However despite this support it hasn’t (yet) been readily adopted.
Support for the initiative is heavily skewed – those who’ve been in healthcare the longest, with perhaps the greatest influence in a command structure, are the least supportive.
These are the results for the same question above when filtered out to surgeons who have worked in healthcare for more than 20 years:
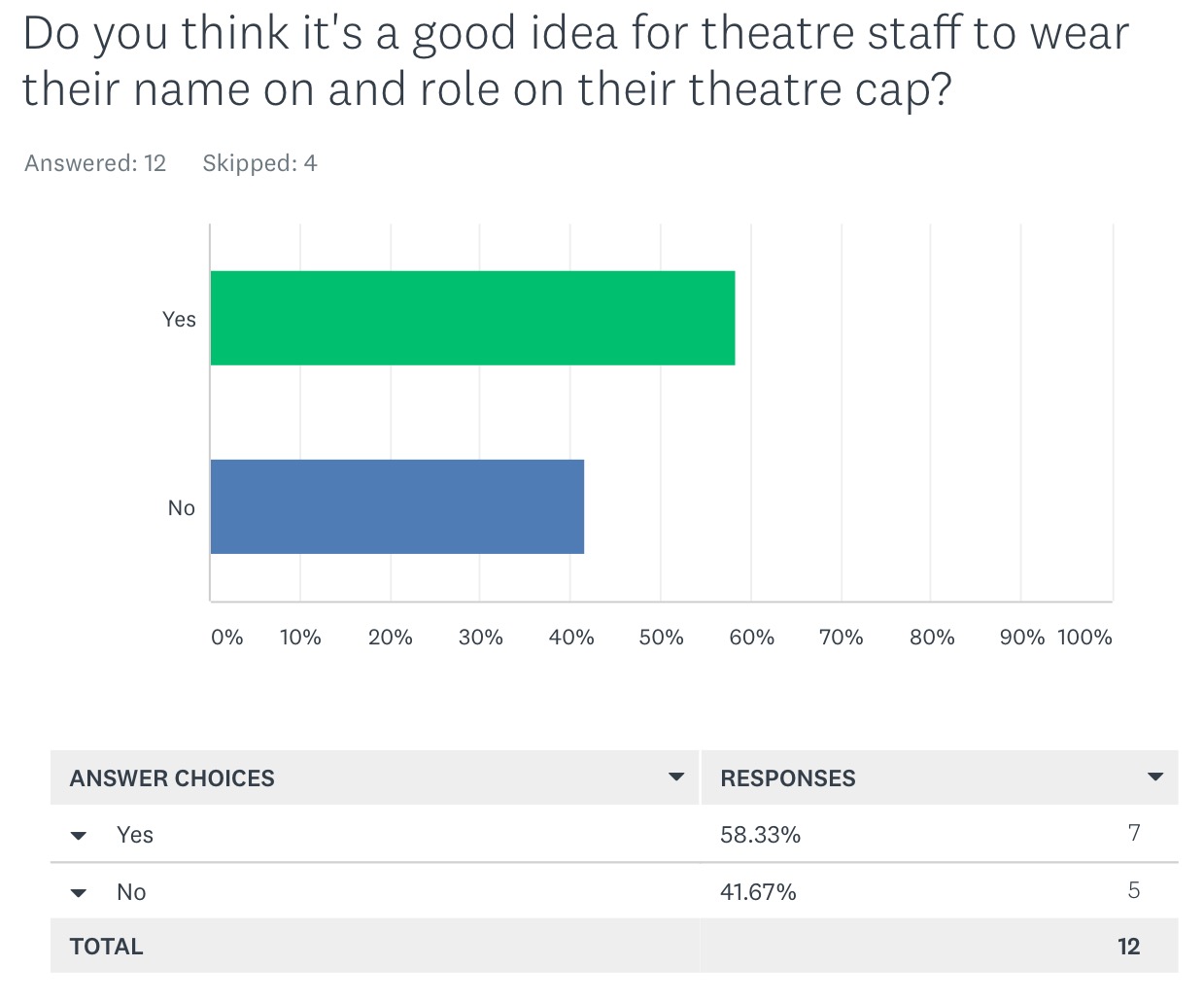
This phenomenon is understandable – perhaps it’s more upsetting for them to acknowledge they could have been doing a better job all this time through a simple intervention. Perhaps they may never accept it such is the power of cognitive dissonance.
Compare the above results with those from nursing & medical students:
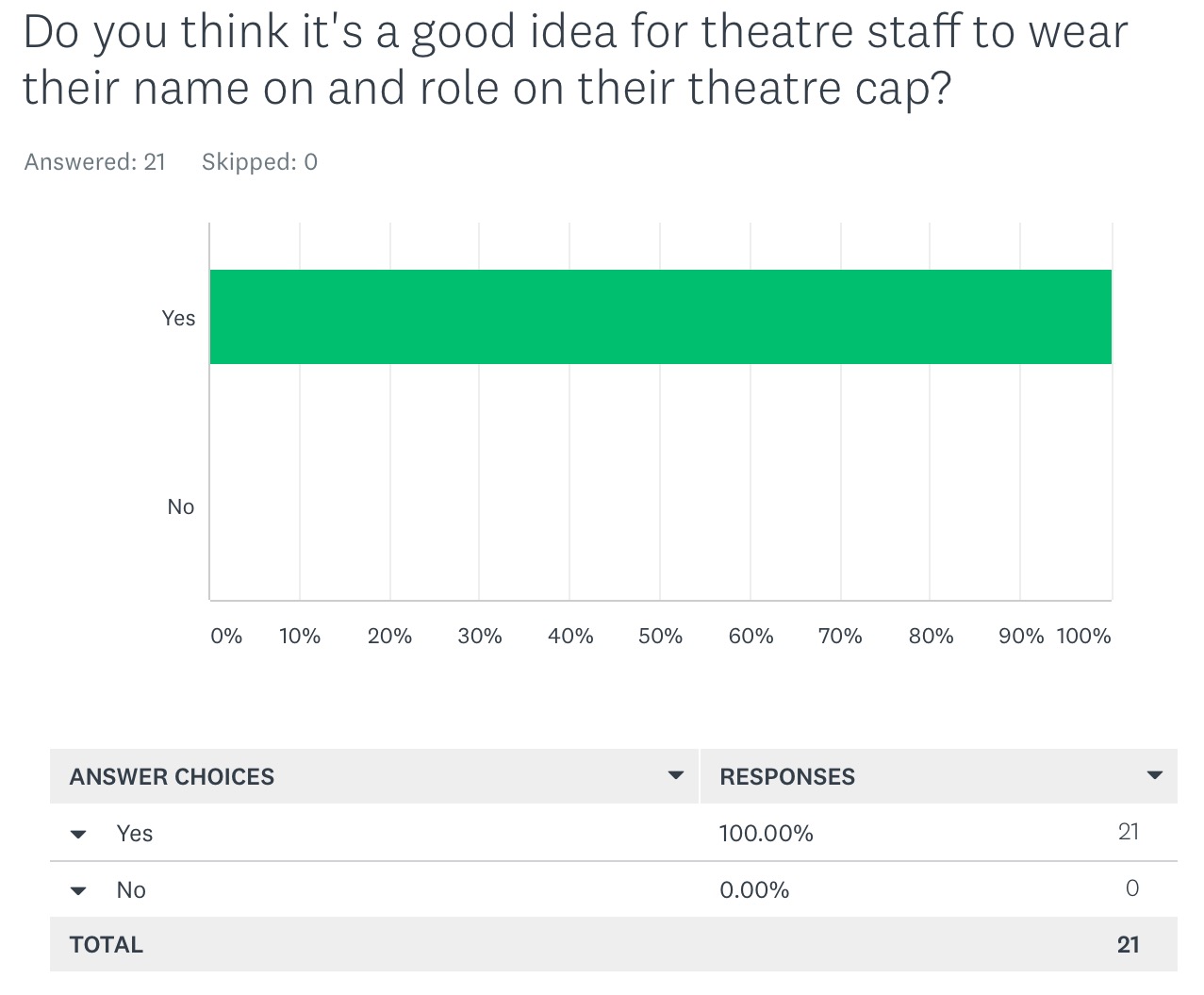
Change and improvement is easily stifled by the influential few in a command structure – unfortunately it is our patients and front line staff who suffer.
Things aren’t all bad. To reach a tipping point, and see a change occur universally one only requires the initiative to be adopted by 25% (see here). However anything less and the initiative will fail. There are a few useful tools to help reach the 25% milestone and we’ve witnessed them playing out on social media – NHS trusts competing against one another to see who has the most staff wearing name & role hats (great to see the NHS leading the way on their 70th birthday). This map clearly demonstrates the impact this friendly competition has had:
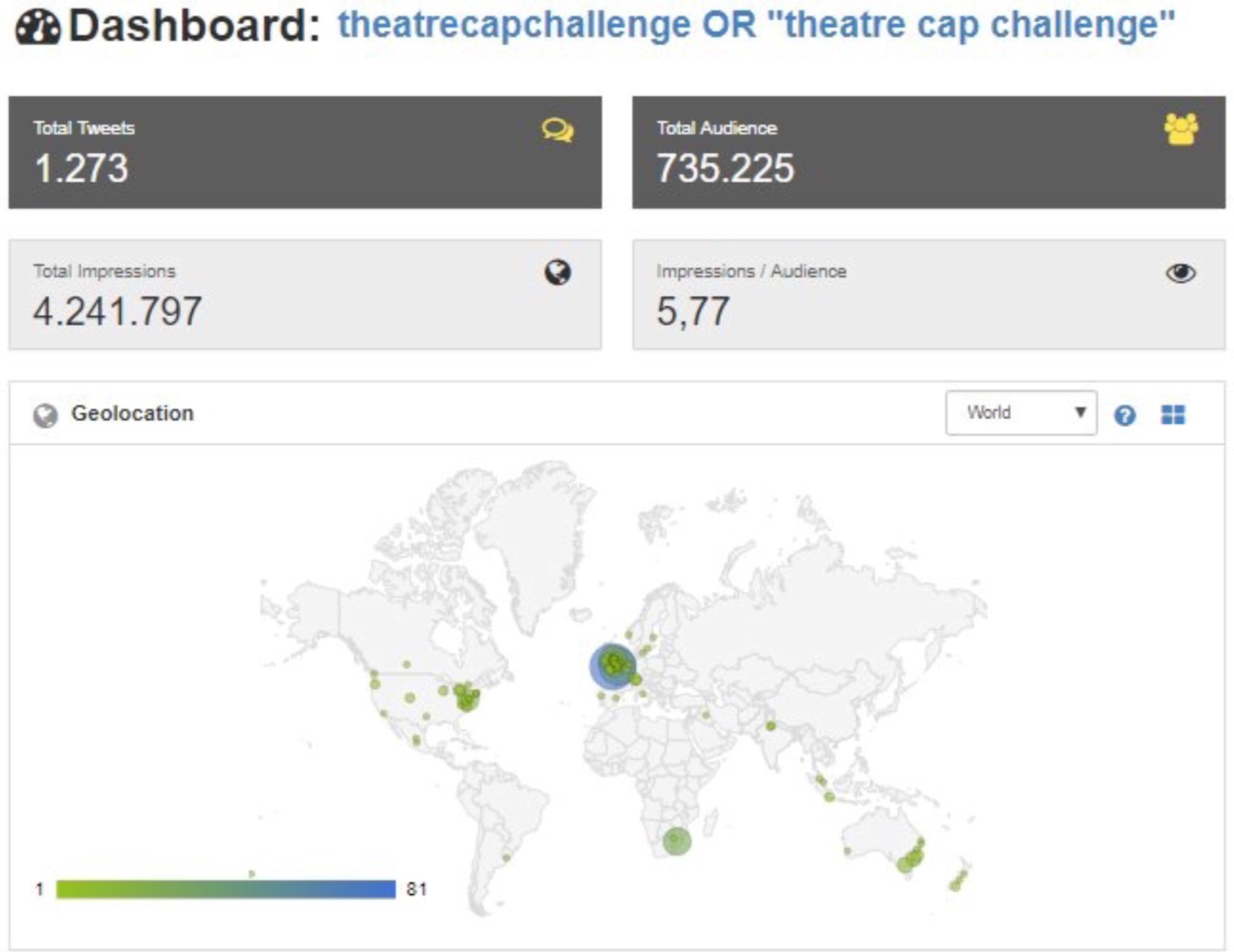
Get 25% of your theatre staff wearing name and role theatre hats and the change is on. Perhaps a great day to focus on making this happen – 23rd July – international #hellomynameis day.
While authoritative command structures readily stifle change they are extremely useful for delivering other things and have demonstrated this for centuries. Increasing efficiency in simple systems, problem solving, education, disciplining……
However, except for rare instances (see here) they struggle to deliver the improvements required to make our front line environments simpler and safer to interface with for patient safety.
For these patient safety interventions to be delivered we would be better served by transparent networked frameworks – a Team of Teams – which more readily seek and develop solutions in complex environments. These structures are leadership driven – where anyone with a passion to drive improvement can help in delivering it.
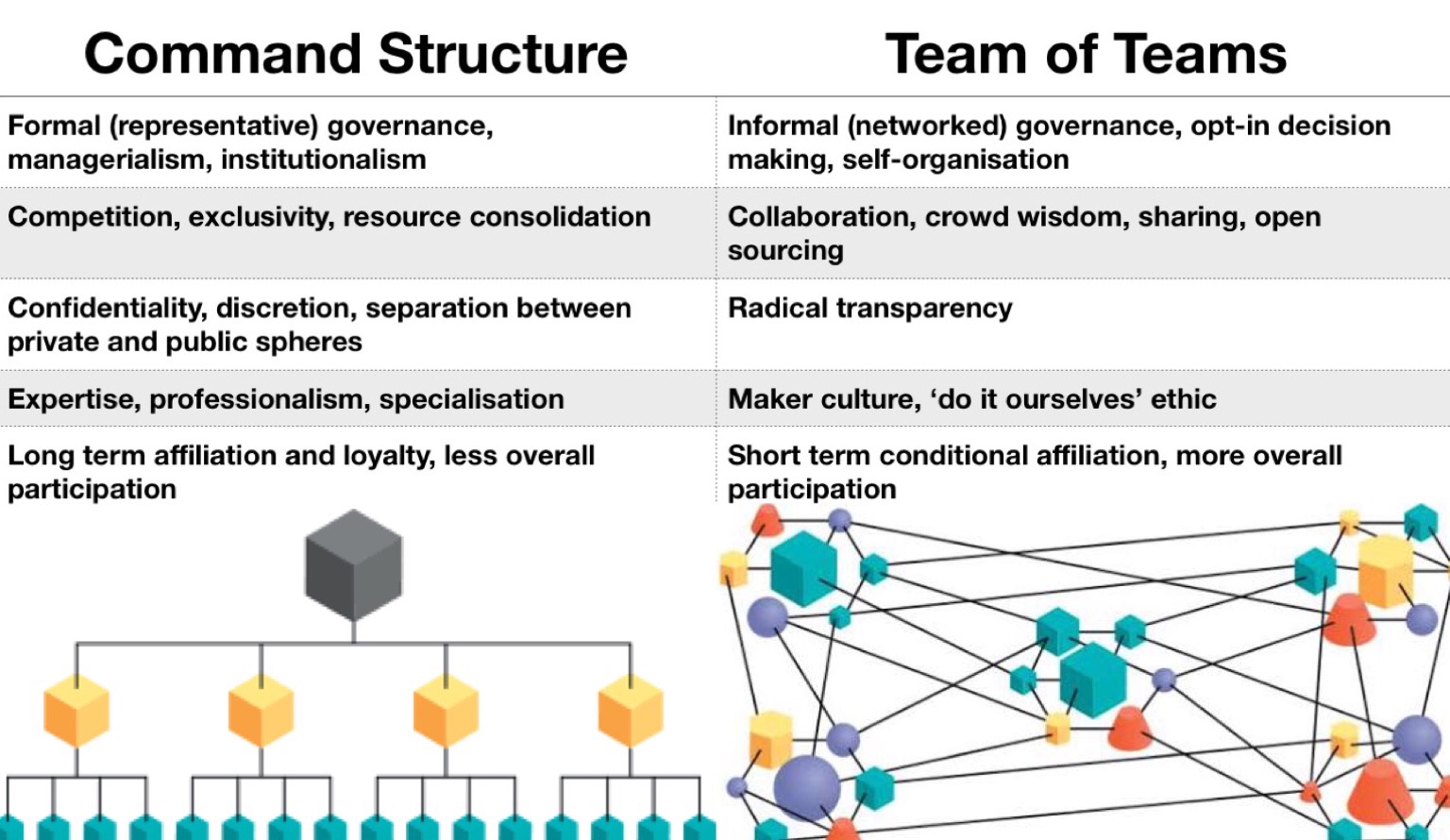
For a Team of Teams to flourish those in managerial positions need to transition from being the voice of authority and instead act as facilitators of front line driven initiatives.
For patient safety to improve healthcare needs to utilise Command and Team of Teams frameworks in harmony with one another.
For this to happen, to break free of the group think, perhaps we’ll need to get our thinking caps on.

Subnote:
Interestingly interventions which make our work environments more complex may be more readily supported as they provide our peers with a competitive edge (after 15 years of data and 4000 studies there is insufficient evidence of patient benefit in using surgical robots which cost millions. However in some environments they’ve been more readily adopted than name & role hats which are essentially free and obviously improve communication and teamwork for patient benefit). A hospital may promote its reputation through having a robot – lay people incorrectly perceiving it represents a modern forward thinking institution.
For patient safety to improve we need a hospitals reputation to be based on providing the optimal environment for patient care – as judged by those best understand it – primarily front line staff. The NHS is leading the way through a subjective leaderboard which scores hospitals based amongst other things upon ‘the percentage of staff who feel able to contribute towards improvements at their trust’ (see here) perhaps we can make this league table more objective.
While we train our medical and nursing staff to be as good as they can possibly be if we continue to make the environment they work in increasingly complex then we will increasingly fail.
It’s time for change.


5 Comments