
Pre-oxygenation is a vital part of airway management immediately prior to intubation and any situation where airway control is taken away from a patient.
We often overestimate our ability to predict airway difficulty – in one study of 3991 difficult intubations 93% were unanticipated (see here). Further the NAP4 study has revealed that airway difficulty is encountered 60 times more frequently in critical care environments than in anaesthesia (see here).
Pre-oxygenation should be performed in the best way possible to provide the greatest time for successful airway control before a patient suffers hypoxic tissue damage.
The Difficult Airway Society have generated guidelines discussing pre-oxygenation in detail (see here).
The DAS guidelines stipulate the requirement for a face mask seal: ‘De-nitrogenation can be achieved with an appropriate flow of 100% oxygen into the breathing system, maintaining an effective face-mask seal’.
Non-rebreather masks (NRM) do not provide a face mask seal. The use of NRM for pre-oxygenation appears to be a culture in some emergency departments. In changing this culture we may provide our patients with a significant increase in the safety of their care.
It is concerning that there appears considerable deviation away from recommended practice. This is of significant detriment to patient safety and warrants further review.
There are a number of disadvantages to using an NRM compared to using face masks which allow a seal:
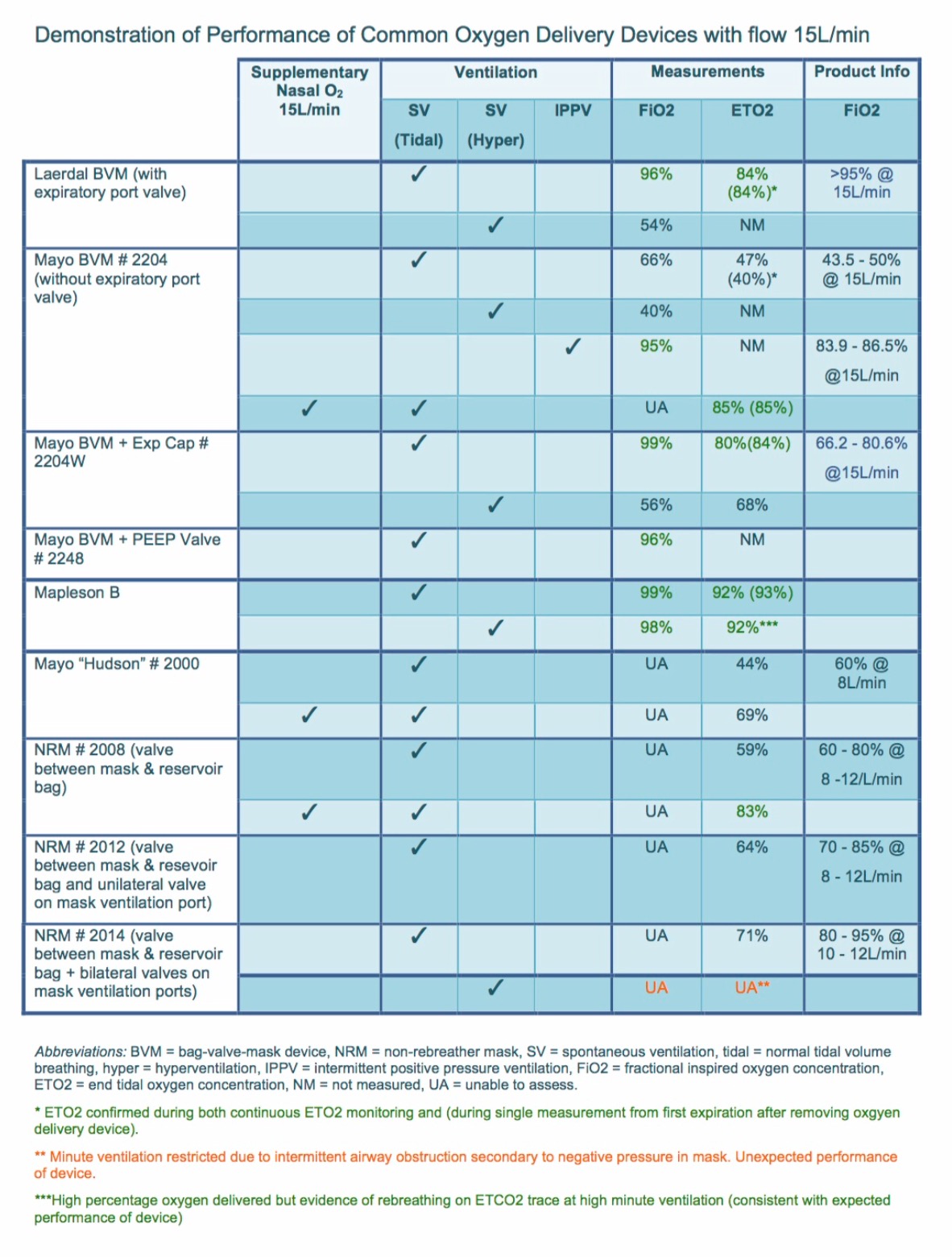
1. The efficacy of an NRM (even with supplemental nasal prong oxygen) for pre-oxygenation is significantly less than that with masks which allow a seal. An NRM is not designed to create a seal on the patient’s face. As a result air is likely to be entrained decreasing the amount of oxygen delivered to the patient. Click image below for study comparing modes of pre-oxygenation by Groombridge et al:
Click on the image below for a further study looking at similar outcomes by Hayes-Bradley et al:
2. An NRM does not offer a means of ventilation
– A device which allows ventilation will be required after the airway has been established.
– A means of ventilation will also be required in the event that intubation is unsuccessful – if a BVM has been used for preoxygenation it is immediately available and checked should this need eventuate.
– The DAS guidelines state that for RSI ‘mask ventilation with 100% oxygen should begin as soon as possible after induction of anaesthesia.’ The benefits of this are huge: (i) maintaining oxygenation (ii) knowing whether or not the patient is mask ventilatable at low pressures prior to intubation. These benefits often outweigh the risks of aspiration which also need to be taken into account. The anxiolytic effect on proceduralists of both of these benefits must not be underestimated – allowing clearer thought processes in an often stressful situation.
3. An NRM is an additional (and may be an unnecessary) piece of equipment which needs to be obtained in an often stressful situation. Additional equipment adds increased complexity detracting focus from the job at hand.
4. Often patients requiring intubation in emergency settings have a decreased level of consciousness and are at risk of airway obstruction. When using an NRM, for reasons discussed below, this obstruction may go unrecognised – the patient may be receiving no oxygen at all through the obstructed airway.
5. The leak around an NRM impairs gas sampling when gas sampling is used (and it should be). The DAS guideline states: ‘De-nitrogenation can be achieved with an appropriate flow of 100% oxygen into the breathing system, maintaining an effective face-mask seal until the end-tidal oxygen fraction is 0.87–0.9’. This indicates the need for an oxygen gas analyser to assess adequate oxygenation prior to induction.
6. To overcome the lower FiO2 from air entrainment around the NRM those who use this technique try to compensate for this by delivering even greater flow rates. This high flow of gas into the mask further impairs gas sampling.
7. Using extremely high oxygen flows in environments where oxygen supply is finite can lead to oxygen supply depletion – patients are then left without oxygen for resuscitation.
8. Gas sampling of both oxygen and carbon dioxide is almost essential to ensure adequacy of pre-oxygenation. Many emergency departments have capnography, most do not have oxygen analysers. There is a possibility they may not be delivering oxygen to the patient at all – it is not uncommon for staff to forget to connect the gas tubing to the oxygen source. Further there have been numerous reports of oxygen pipeline failures and crossovers (see here) – in one emergency department over 300 patients received nitrous oxide instead of oxygen before this issue was noticed – unfortunately by this time 27 patients had died as a result. This is not an issue which has been relegated to history, pipeline crossovers occur regularly and continue to cause unnecessary deaths throughout the world.
Perhaps the lack of oxygen analysers in particular environments has allowed a culture of pre-oxygenation with an NRM to persist in these departments. Without sufficient feedback we rarely improve.
Please note – pulse oximetry alone provides very poor feedback on the efficacy of pre-oxygenation or airway maintenance. The majority of patients oxygen saturations will be close to 100% despite no pre-oxygenation. There is also a significant delay between loss of oxygenation and a change in oxygen saturations. This makes the use and feedback obtained from oxygen analysers and capnography of even greater importance.
Further NAP 4 has shown us that airway difficulties are 60 times more common in critical care environments than anaesthesia making oxygen analysers and other other optimal equipment even more important.
9. Disconnecting oxygen from an NRM to the device required for ventilation requires an additional unnecessary step.
10. Disconnecting a gas sample line from an NRM to the device for ventilation requires an additional unnecessary step. Any additional steps increase complexity in what is often a staff limited and stressed environment.
Dr Nicholas Chrimes discusses the principles of pre-oxygenation in more detail (see here).
Please note that the assessments performed by Dr Nicholas Chrimes have been carried out on healthy patients where a patent airway is guaranteed.
Often when patients are intubated in ED it’s because of a threatened airway – the airway is dynamic and may potentially obstruct during the preoxygenation phase – this is readily recognised when waveform gas analysis is used. Where it is not, for example with a non rebreather, airway obstruction may mean the patient is not receiving any oxygen at all. Where it is, for example with a face mask seal, attempts can be made to rapidly open the airway, with great feedback as to whether this has been done, and ventilatory support be provided immediately pending intubation.
Reasons provided for use of an NRM for pre-oxygenation have included:
A. ‘Holding a Bag Valve Mask or Mapleson Circuit for pre-oxygenation requires a level of skill that the person managing the airway may not have’. Holding a mask that obtains a seal is not a difficult skill to obtain particularly with the feedback of gas analysers. This skill should be one attained by any staff member given charge of looking after a patient’s airway.
B. ‘Using a non-rebreather mask frees the staff member up to perform other tasks’. There is much that needs to be done in the period prior to intubation – staff and equipment readied and checked. If the staff numbers are insufficient to dedicate an individual solely to provide preoxygenation at this time then an NRM may be suitable while the environment is readied. However in the period immediately prior to induction optimal preoxygenation needs to become the primary focus at this time – change from the NRM to a face mask seal and ensure preoxygenation is performed optimally.
C. ‘Patients may be intolerant of a mask with a seal on their face (they may be claustrophobic)’. There are many methods to help overcome this issue including having the patient hold the mask themselves, sedating the patient, holding the mask increasingly close to the patient as they become more sedated eventually attaining a seal…. This certainly is not a reason for an NRM to be used routinely for pre-oxygenation. Administering a small dose of induction agent, in effect sedating the patient, will likely allow them to tolerate the mask and where a face mask seal (e.g. BVM) then one is immediately able to ventilate the patient should the patient become ‘over’ sedated.
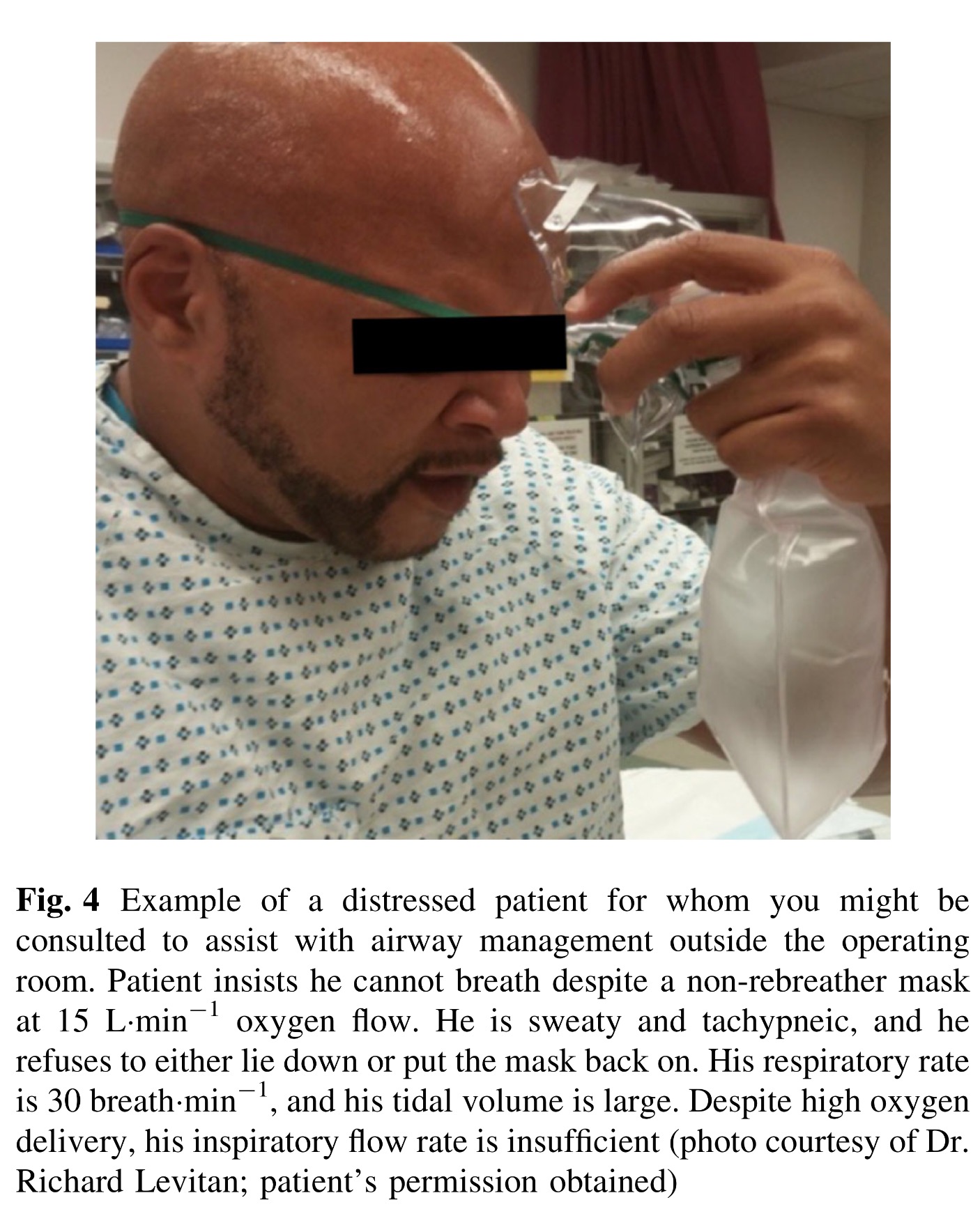
Perhaps one might be more likely to keep a mask on a patient when you are holding on to it.
D. ‘There is an increased work of breathing when a patient is spontaneously breathing using a Bag Valve Mask’. The picture below demonstrates that the inspiratory valve of a laerdel bag is already open without any effort from the patient when an oxygen flow of 15L/min is delivered into the bag.

We will note there was a decrease in ease of breathing noted by patients in Groombridge’s study when using BVM compared to NRM.
There is misunderstanding by some doctors that the bag of a BVM needs to be squeezed to deliver oxygen to the patient (leading to further inappropriate concern that has will then be insuflated into the patient’s stomach increasing the risk of aspiration) – as can be seen from the image above this is not the case.
E. An historical and potentially detrimental belief by some is that mask ventilation is absolutely contraindicated in the phase of rapid sequence induction between administration of induction drugs and patient apnoea up until the time of intubation.
There is a real risk of aspiration during this phase and insufflation of the stomach will increase this risk – however low pressure mask ventilation (below barrier pressure) in those with an intact lower oesophageal sphincter and/or no significant history of reflux should not increase this risk significantly. Low pressure mask ventilation is easier to attain with an anaesthetic circuit with an adjustable pressure limiting valve set for example to 15cmH2O – this may not be readily available in emergency departments.
Their is great value in mask ventilation during this phase which should not be underestimated for two main reasons:
(i) oxygenation is maintained
(ii) an assessment is made as to whether a patient can be ventilated at low pressures which impacts on the consideration that the patient cannot be intubated. If they can be mask ventilated this relieves the intubator of a vast amount of psychological pressure and naturally they become more relaxed and are able to think more clearly in a calm manner. If the patient can’t be mask ventilated at low pressures the intubator can already be considering the need for additional airway adjuncts (Guedel, LMA etc) in the event that they cannot intubate the patient.
This article from Canadian Journal of Anaesthesia (see here) from 2007 discusses each component of Rapid Sequence Induction – see section 8 for a discussion on the benefits of mask ventilation prior to intubation. The use of mask ventilation prior to intubation is also supported by the Difficult Airway Society Guidelines (see here).
G. Proponents of NRM use for preoxygenation discuss ‘overcranking’ the flow meter to deliver >15L/min of oxygen flow. Studies have shown that when ultra high flows of oxygen are used >40L/min into a NRM then similar FiO2s may be reached to those delivered with a face mask seal (see here). However these results must be extrapolated with caution to the clinical population. Use of high oxygen flowrates is suboptimal due to unregulated/measured flow and some flowmeters do not allow these flow rates. Sometimes the pressure generated by these high flows causes the oxygen tubing to pop off. It has been shown that oxygen flowmeters in Australia do not provide flow rates of greater than 19L/min (see here) and subsequently do not provide optimal FiO2 (see here).
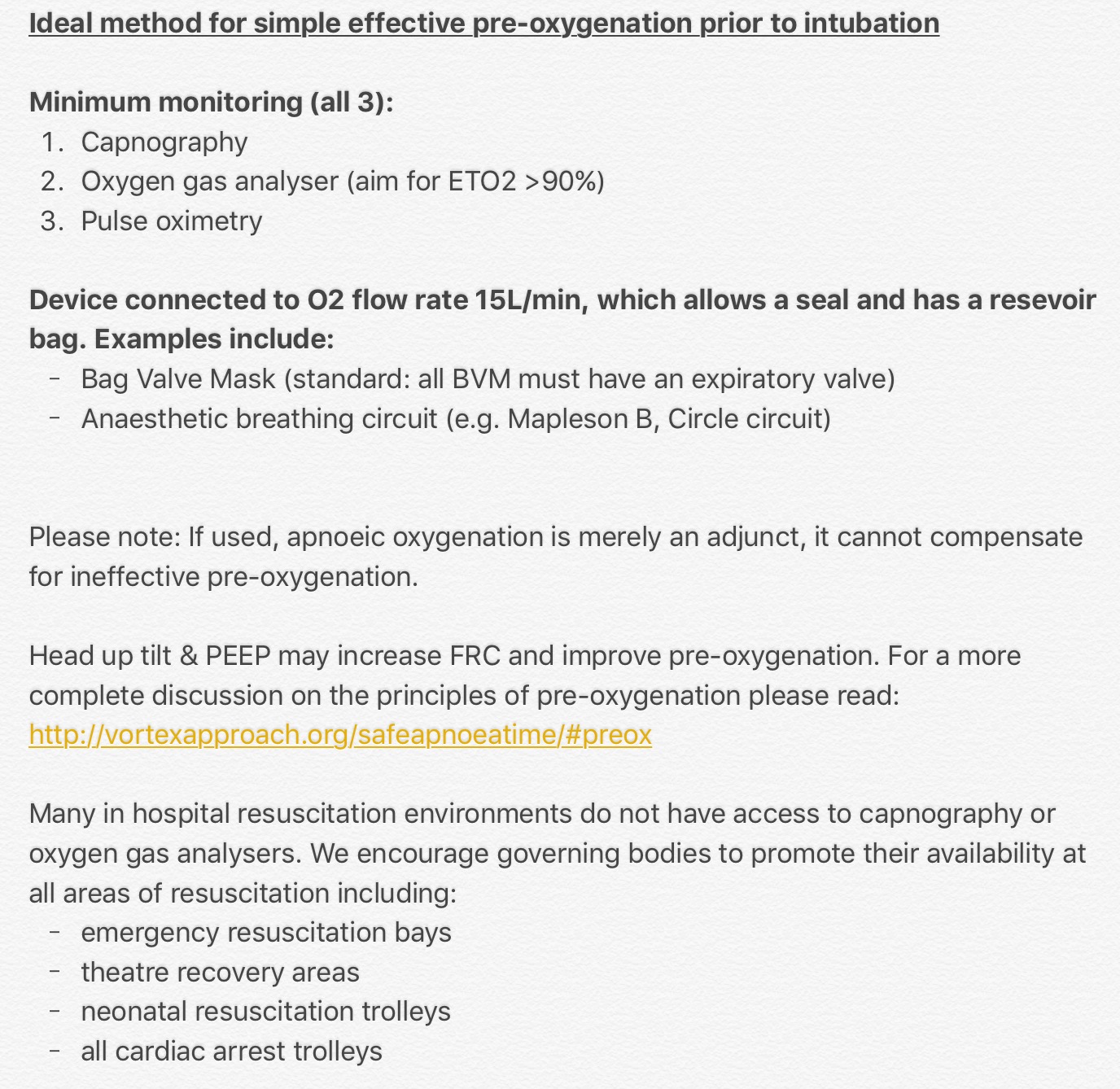
Perhaps the outline below, based on the DAS guidelines and input from several experts in airway management, represents a simplified approach to optimal pre-oxygenation:
Please forward this on to others for discussion and support the introduction of gas analysers in all areas of resuscitation (see here). While conditions may vary with patient, physician and environment it is vital that we understand and adopt the best approach to pre-oxygenation for optimal patient care.
The culture of NRM use for pre-oxygenation seems to be particularly prevalent in emergency departments in the United States where emergency physicians primarily manage patients airways. This culture may have existed for some time. It may also have been perpetuated by several dedicated, respected and influential emergency physicians (see here):
We ask that they work with anaesthetists and other experts in airway management to review their recommendations to ensure an optimal approach to pre-oxygenation.
It is time to stop the culture of non-rebreather mask use for routine pre-oxygenation and limit its use to those rare cases where it may be beneficial (e.g. in cases where it’s impossible to obtain a face mask seal and there is no access to THRIVE)?
Further it has come to our attention that in some countries BVMs do not come with an expiratory valve as standard. BVMs without an expiratory valve will entrain air during spontaneous ventilation during preoxygenation significantly impairing preoxygenation. We are working with airway experts to create a list of BVMs with and those without expiratory valves (see here).
Thank you.
Below we provide several tweets from physicians and paramedics expressing concern about the use of NRM for pre-oxygenation:




7 Comments