Do the ACORN Standards in relation to theatre caps cause unnecessary environmental, financial and patient harm?
Should we find better rules based on the best available evidence and developed through collaboration to provide better patient care?

’A few years ago, the Dean of the School of Business at the University of Leicester, Dr Zoe Radnor, tried to understand the reasons for the “bicycle book” that she discovered at an English hospital she was studying. All staff who arrived at work by bicycle routinely signed a register book at the front door. Hundreds of these registers, once full, had been collected and stored for decades in clearly marked boxes. “Why?” Professor Radnor asked. No one knew.
The answer took some sleuthing. The first books dated from World War II—when rationing of fuel was the rule of the day, and when any staff who commuted by bicycle thereby earned extra food ration credits for saving on gas. Now, three-quarters of a century later, the bicycle book process remained alive and well, embedded in the organization’s brainstem, not its cortex. It was pure waste.’ (1)
(From – Breaking the rules for better care. Donald M. Berwick et al)
Practices maintained through a command structure often go unchallenged. They can be perpetuated and reinforced for years.
When this phenomenon persists against our best interest then these ‘rules’ need to be either changed or broken.
Within Australia many institutions use ‘ACORN Standards’ to defend their insistence on the use of disposable theatre caps:
‘ACORN have decreed that linen theatre caps are no longer acceptable, for infection control reasons. I think this is silly, and I don’t know why they think they are the sole determinant of what goes on in theatres; but I am not going to win that battle.’
‘VMO in infectious disease rang to say hats are not permitted! ACORN says they must be washed at 85 degrees and ironed…’
‘Just wanted to share/vent my experience at XXXXX. I went there for the first time in 4 months today. Wore the named cap. As I walked through the corridor for the first time, the theatre NUM comes to me and says that it is hospital policy to only wear disposable caps! So she gave me one to put over the top. I asked why. “Because its our policy”… I didn’t kick up a fuss. But I am frustrated by bureaucratic rules which have little or no evidence backing!’
‘I sympathise with your frustration. I have similar objections where I work in Australia. The problem here arises largely from a Perioperative Nursing Association (ACORN) that has produced guidelines which include a section on appropriate perioperative attire. It is that document which managers here quote when objecting against cloth or laundering services.’
‘How did you overcome resistance to reusable hats from DONs quoting ACORN standards and no evidence of daily/adequate laundering’
For a fantastic, in depth, review of the ACORN Standard please read ‘A challenge to cloth theatre caps’ by Dr Rhys Thomas – Quality and Safety Fellow. (2)
In May 2018 ACORN released a position statement defending their standard in it’s existing format. (3)
Primarily it indicates:
‘Personnel have a duty to demonstrate that cloth head covers meet the relevant Australian standards for perioperative attire textiles, labelling and laundering.’
Further:
‘The development of these standards is not governed by ACORN and thus ACORN cannot change their content.’
It is of great importance that people are aware the Australian Standards ACORN reference in their own standard do not relate to headwear:
AS/NZS 1957:1998 ‘Textiles – Care Labelling (4)
‘Goods exempt from Care Labelling Requirements: Unsupported coats (including overcoats, jackets and the like) of PVC film, handkerchiefs, braces, garter suspenders, arm bands, belts, headwear.’
AS/NZS 3789.3:1994 ‘Textiles for health care facilities and institutions – Apparel for operating theatre staff’ (5)
‘This Standard specifies requirements for the finished dimensions, materials and manufacturing of apparel for operating theatre staff. Items of apparel include theatre dresses, two-piece suits, warm-up gowns, warm-up jackets and theatre boots.’
Given these Australian Standards do not relate to theatre hats reference to them by ACORN in relation to their policy on cloth headware is unwarranted.
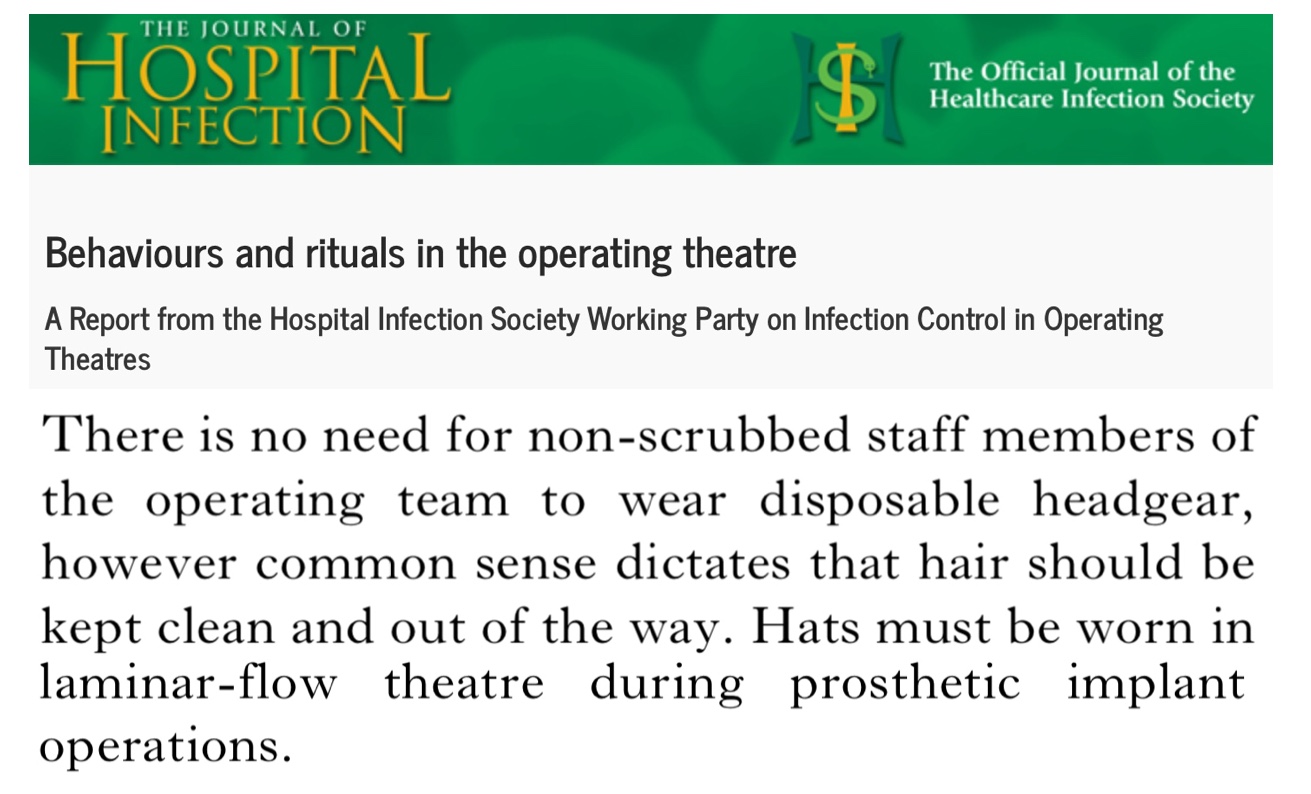
Further all available evidence to date (and there is much) demonstrates no difference in surgical site infection rates when comparing reusable versus disposable theatre hats:
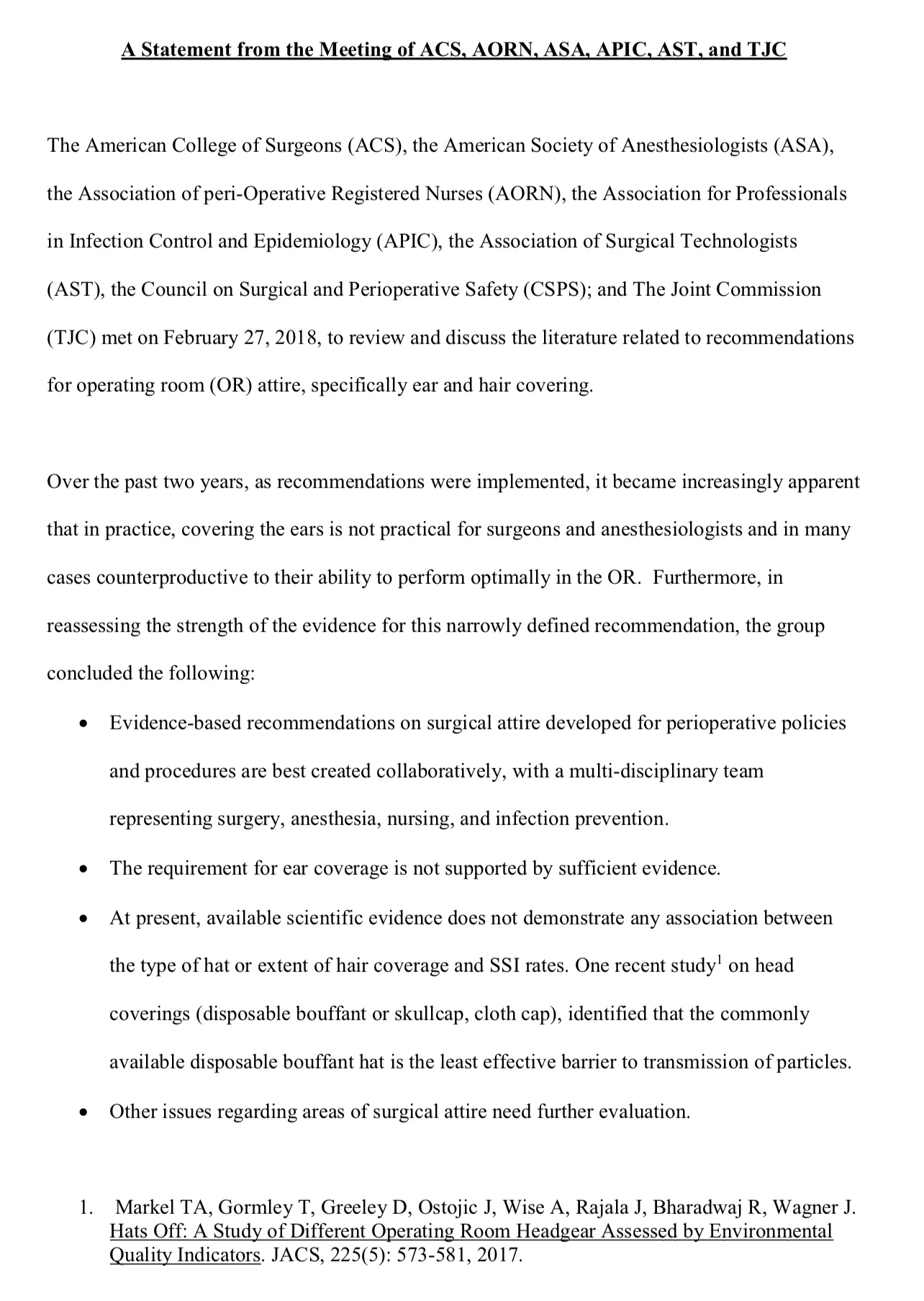
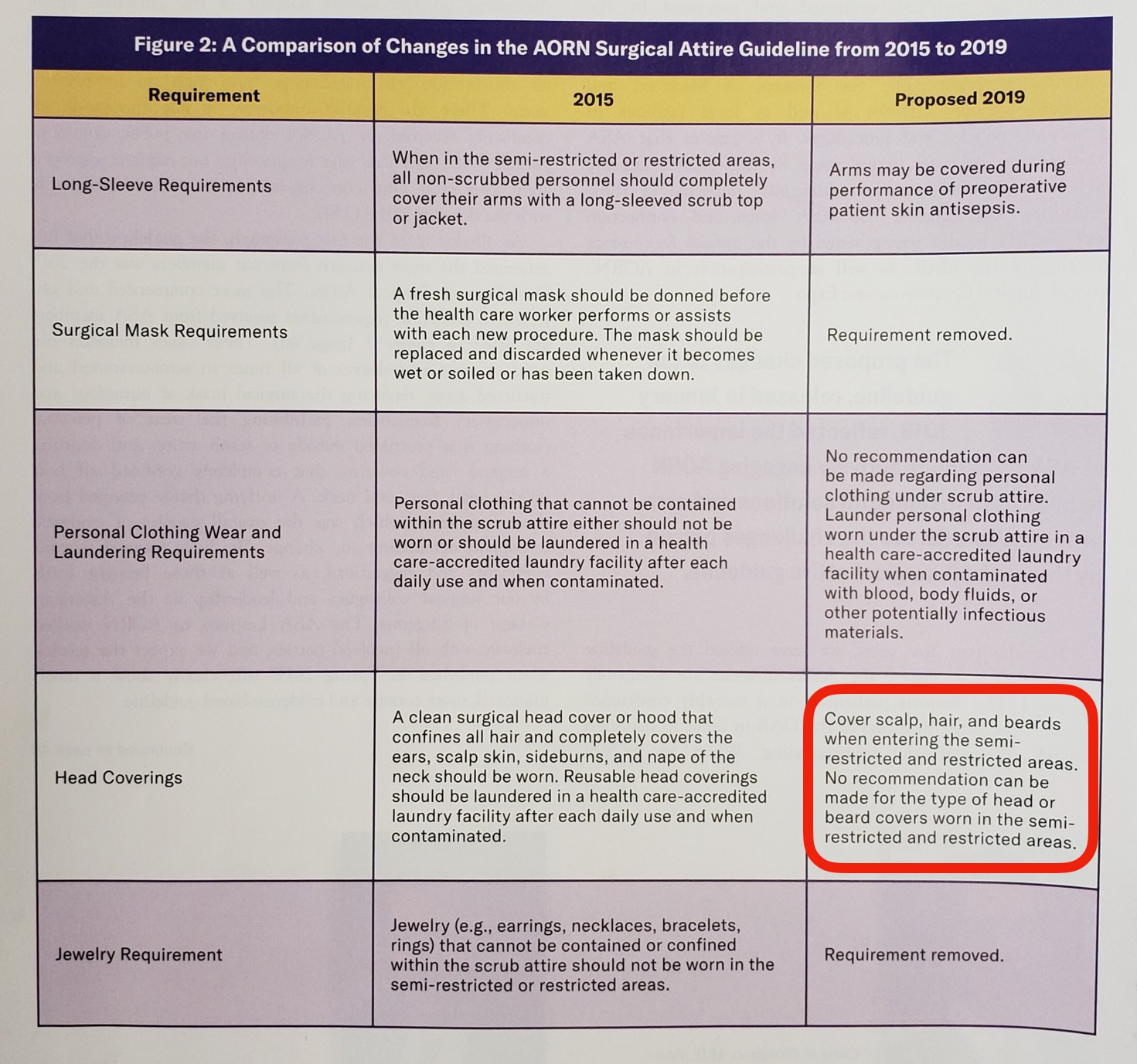
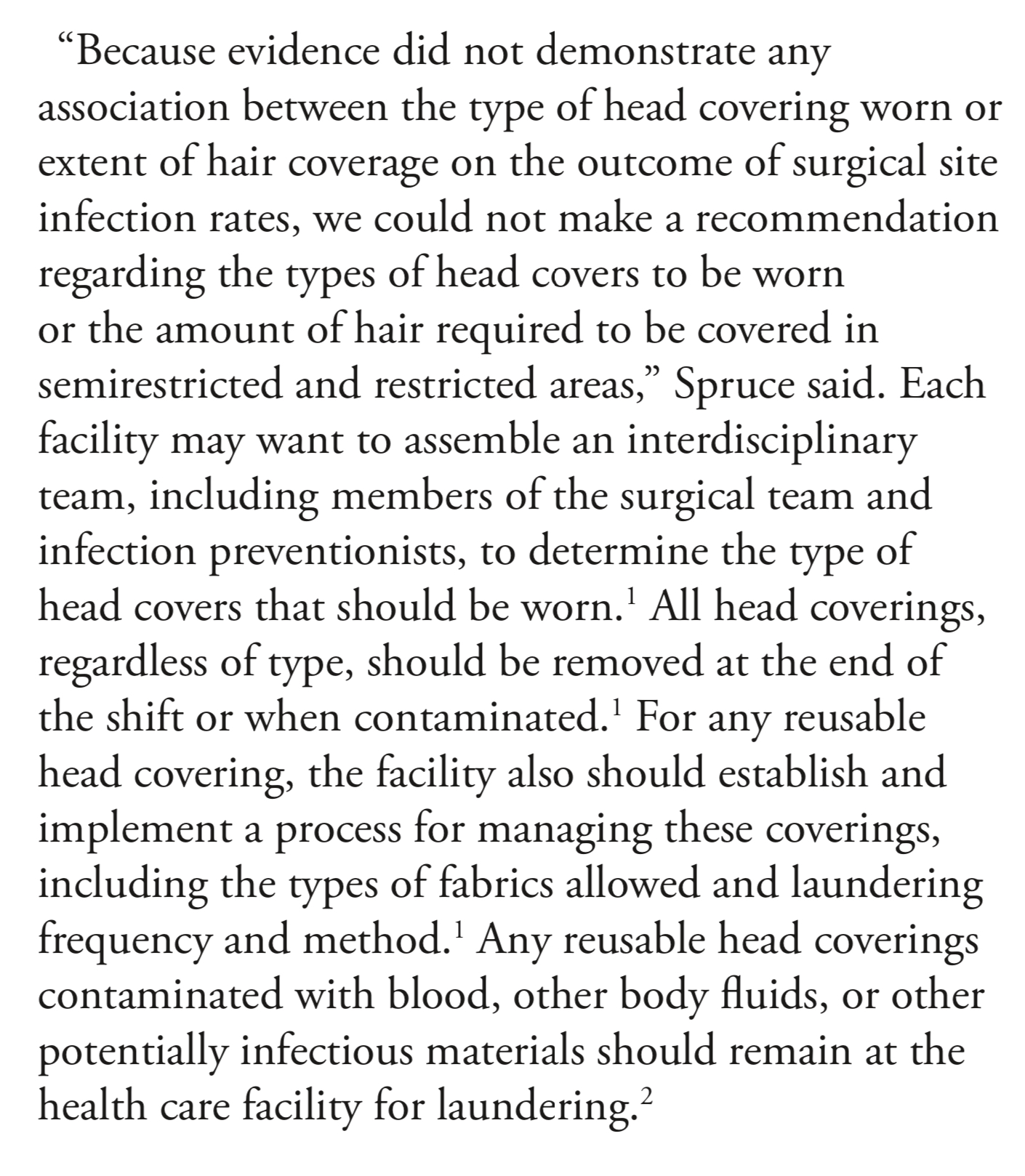
Within America the ACORN equivalent, the AORN, recently released a collaborative statement with several other healthcare authorities taking into account the available evidence: (11)
Perhaps it would be wise for us to follow evidence based standards developed through collaboration with the AORN to provide a better level of care.
For those looking for guidance on best practice for home laundering of reusable theatre caps these guidelines provided by Mrs Scarlett McNally from the Royal College of Surgeons appears the most sensible given the available evidence. In summary:
Within Australia, mandatory disposable hat use driven by institutional interpretation of the ACORN standards is not supported by evidence however it does cause significant detriment financially, environmentally and to patient care.
Financial Cost
From – Operating Room Attire Policy and Healthcare Cost: Favoring Evidence over Action for Prevention of Surgical Site Infections. Almouhsly A. et al. Journal of the American College of Surgeons. October 2018:
‘Implementation of the AORN guidelines (2015) has not decreased SSIs yet increased healthcare costs. The cost of attire for 1 person entering the operating room increased from $0.07 to $0.12 before policy change to $1.11 to $1.38 after policy change. Use of the mandated operating room long-sleeved jackets alone in our institution was associated with an added cost of $1,128,078 annually, which translates to an estimated $540 million per year for all US hospitals combined. (12)
Environmental Cost
It is estimated that a 20 theatre hospital discards over 100,000 disposable hats every year. Disposable theatre hats are made from viscose whose production is particularly harmful to the environment. (13)
The Australian and New Zealand College of Anaesthetists actively support the use of reusable hats in their Statement on Environmental Sustainability in Anaesthesia and Pain Medicine Practice – PS64: (14)
Patient Care
Reusable theatre hats represent the best location for name and role identification taking in to account the work flows of front line theatre staff.

Name and role identification is associated with improved communication, teamwork, staff engagement, theatre efficiency and clinical outcomes. (15)
The Garling Enquiry 2008 stipulated that all healthcare staff clearly display their name and role. (16)
An institutions insistence on disposable hat use based upon interpretation of ACORN standards hampers this stipulation.
It is worth noting that ACORN standards are not upheld by legislation – ACORN are a health promotion charity – they produce high quality standards and as such are looked towards in helping guide best possible practice.
Reviewing the ACORN standard as related to theatre hats, collaboratively and through assessing the available evidence, will demonstrate ACORN is positioned to continue to guide best possible theatre practice in the future.
I’m fortunate to work in several institutions which allow reusable hats. I also work in several which don’t – I still wear reusable hats there as well.
While rules persist against our best interest perhaps it’s in our best interest to find better ones or simply to break them.
I’d be delighted to hear your feedback on this issue.
References
- Breaking the rules for better care. Donald M. Berwick et al
- A challenge to cloth theatre caps. Dr Rhys Thomas
- ACORN Position Statement on Cloth Headware
- AS/NZS 1957:1998 ‘Textiles – Care Labelling
- AS/NZS 3789.3:1994 ‘Textiles for health care facilities and institutions – Apparel for operating theatre staff’
- Is there an association between surgeon hat type and 30-day wound events following ventral hernia repair? Haskins IN, et al. Hernia. 2017.
- Mandatory Change From Surgical Skull Caps to Bouffant Caps Among Operating Room Personnel Does Not Reduce Surgical Site Infections in Class I Surgical Cases: A Single-Center Experience With More Than 15 000 Patients. Hussain S, et al. Neurosurgery, Volume 82, Issue 4, 1 April 2018, Pages 548–554.
- Use of Environmental Air Quality Indicators to Assess the Types of Surgical Headgear Typically Used in a Dynamic Operating Room Environment.Markel T et al, Journal of the American College of Surgeons. October 2017. Volume 225, Issue 4, Supplement 2, Pages e29–e30
- Bouffant vs Skull Cap and Impact on Surgical Site Infection: Does Operating Room Headwear Really Matter? Kothari SN, et al. J Am Coll Surg. 2018.
- Operating Room Attire Policy and Healthcare Cost: Favoring Evidence over Action for Prevention of Surgical Site Infections.Elmously et al. Journal of the American College of Surgeons. 2018.
- A statement from the meeting of ACS, AORN, ASIC, ASA, AST and TJC.
- Operating Room Attire Policy and Healthcare Cost: Favoring Evidence over Action for Prevention of Surgical Site Infections. Almouhsly A. et al. Journal of the American College of Surgeons. October 2018.
- Viscose – material guide
- ANZCA Statement on Environmental Sustainability in Anaesthesia and Pain Medicine Practice – PS 64.
- #TheatreCapChallenge – Where’s the Evidence?
- Final Report of the Special Commission of Inquiry. Acute Care Services in NSW Public Hospitals. Peter Garling SC. 27 November 2008.


4 Comments