Why bother with an opinion piece – everyone is entitled to their own opinion yet where it disagrees with the opinion of others it creates annoyance.
So perhaps best to keep ones opinion to oneself because we are all very comfortable with the status quo thank you very much.
This week the Royal Colege of Anaesthetists released yet another fantastic National Audit Project – NAP6 on anaphylaxis.
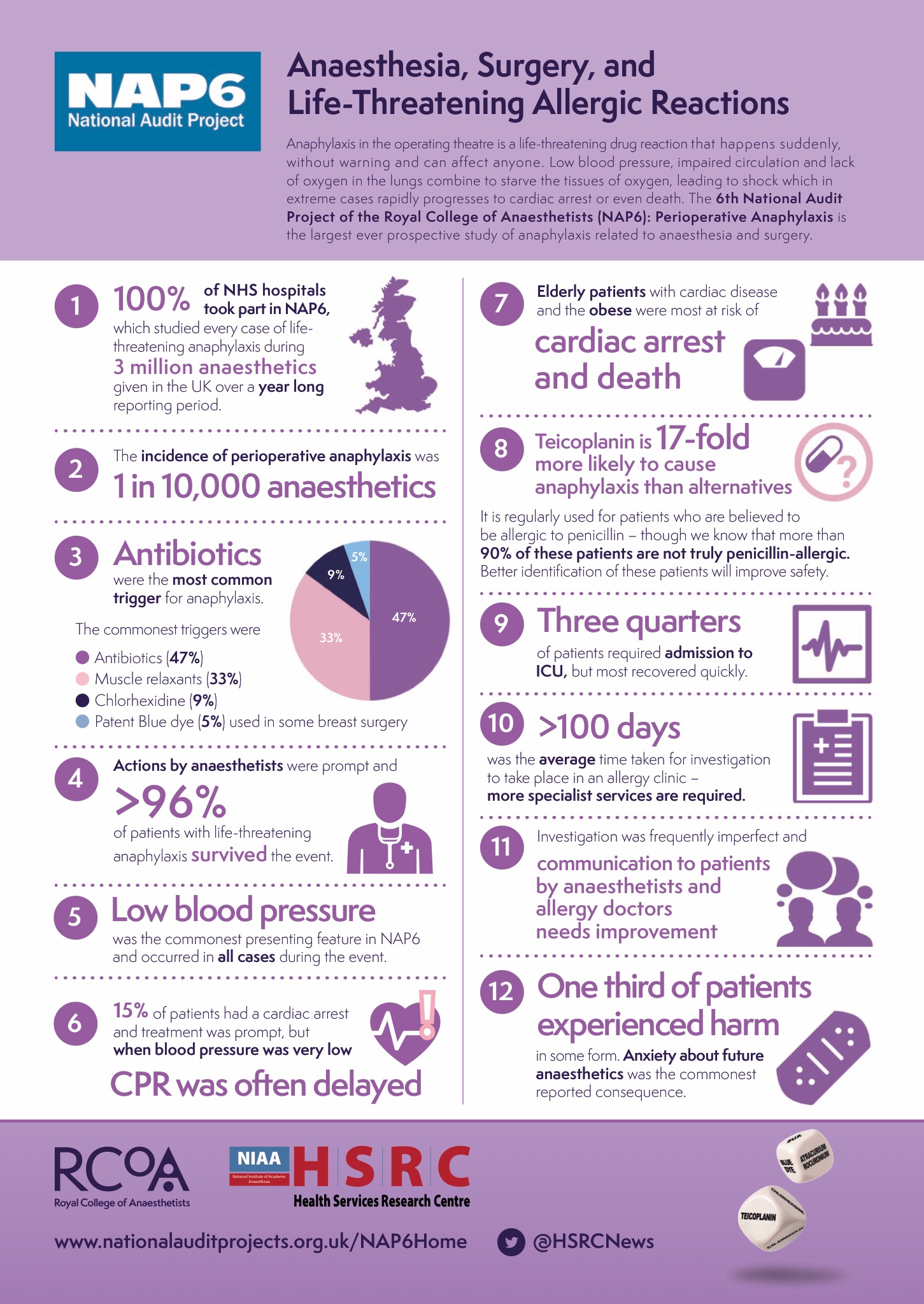
Already I’m biased – I’m from the UK originally, born and bred in the NHS and I love it and all it stands for – yes it has its issues yet I see a very bright future. From memory the NHS is the 3rd biggest employer in the world – at present nowhere else will be able to obtain such amazingly vast data.
A 100% participation rate by hospitals too – where else would get that?
How has the NAP6 data changed my practice:
– If someone asks me to prescribe Teicoplanin then they better have an extremely good reason
– I haven’t used suxamethonium for over 4 years and will raise an eyebrow when I hear my colleagues using it (really – it doesn’t have a lot going for it). I will likely forward them the NAP6 data.
– I will have more discussions with my colleagues about their choice of non-depolarising muscle relaxant. The discussions will likely follow this sort of pattern (well this is my opinion anyway):
Given the ready availability of sugammadex…… (if you don’t have it readily available perhaps look at the foreheads of your colleagues – do they have their names and roles written on their hats? Probably not – this is because you don’t have a great safety culture in your workplace yet – work on it and the sugammadex will be more readily available).
Given the ready availability of sugammadex and its ability to rapidly and effectively reverse rocuronium and vecuronium then these are in my mind really the only 2 choices of NMB agent (unless you don’t want to reverse your patient well or for a long time – pancuronium?)
There appeared to be no cases of vecuronium anaphylaxis in the NAP6 data:
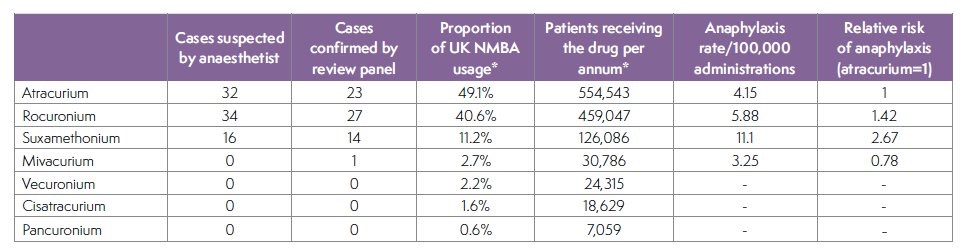
Perhaps this was due to fewer patients being administered the drug when compared to other NMB however it certainly indicates a lower anaphylaxis rate compared to rocuronium. For every 17,000 cases in which I use rocuronium in I should expect a case of anaphylaxis to it (maybe I’ll have one before I retire from clinical work and that patient should have a 96% chance of survival).
One of the conclusions of NAP6 was:

Perhaps they are considering that vecuronium does cause anaphylaxis (we know it does) yet among the 24,315 patients receiving it they didn’t have one.
If we look at data from Western Australia they may have been due a case of anaphylaxis when they had given vecuronium to 35,714 patients:
A further influential article from New Zealand discussing the incidence of anaphylaxis to NMB had significant impact across the ditch. The results it discusses appear to be out of keeping with those of the NAP6 and Western Australia study. From speaking to an expert in allergy testing he believes this difference is likely due to the small numbers and the way that allergy testing is performed in New Zealand. This was one of his comments:
The study had significant impact in New Zealand in affecting NMB choice. Based on the NAP6 data along with the Western Australian data my Kiwi colleagues might consider re-assessing the New Zealand data – I am aware of the consternation this suggestion might cause (perhaps I shouldn’t eat lamb or play Rugby for a while).
It certainly appears that the risk of anaphylaxis from vecuronium is less than that of rocuronium and perhaps the Western Australia data still gives us the clearest idea of the magnitude.
If vecuronium and rocuronium were exactly the same other than their anaphylaxis profile it would be a no brainer – I’d be Using vecuronium – if I could avoid that one case of anaphylaxis in my career I certainly would irrespective of my 95% chance of resuscitating the patient.
However rocuronium and vecuronium are quite different – it’s this difference I’d like to focus on.
This difference – laid bare but undefinable over a vast number of anaesthetics and hidden from view is a wicked problem – perhaps not the best example because there’s some real corkers in healthcare and they’re harming our patients in droves.
What is a wicked problem?
A wicked problem is one that is difficult to solve for several reasons including:
– the interconnected nature of these problems with other problems (eg driving change in healthcare exposes oneself – governing bodies feel safer maintaining the status quo)
– incomplete knowledge (eg lack of communication amongst error reporting systems & poor/no systems for reporting hazards)
– the number of people and opinions involved (eg so many governing bodies in healthcare, often one will pass the buck to another saying we can’t change unless another group changes)
Here’s a great example – the presence of unnecessary Claesen Harness clips on our anaesthetietic masks.

This creates un-foretold pollution to the world given perhaps no one has used a Claesen Harness (other than for historical demonstrations) for perhaps the last 15 years. Who is in charge of getting rid of them when we have so many different levels of governance?
Perhaps another glaring example we’re working to fix is Australian Standardisation of the Hospital Emergency Number (see here – ASHEN). Britain standardised the Hospital Emergency Number across all of its hospitals over 10 years ago at ‘2222’. Europe is looking to follow suit.
From an ongoing survey where we’ve collected data from a third of Australian Hospitals we’ve identified 48 different numbers – embarrassing really given the implications of resuscitation delay through staff not remembering the number.
Let’s make it easier for people to remember by standardising – perhaps that we haven’t already is because of increasing and fractionated healthcare governance and the nature of our error reporting systems.
We have opaque error reporting systems which don’t communicate with one another and only focus on adverse events and near misses. What they don’t pick up well are the hazards – having at least 48 different Hospital Emergency Numbers across Australian Hospitals is a hazard.
We’ve spent so much time focussing on individuals and teamwork and very little looking at the environment we put them in. Perhaps because we’ve felt powerless to improve our environments – certainly current healthcare frameworks struggle to help. We can work differently (see here) – making it easier for people to do their jobs right. The best interventions to support this focus on the systems and equipment we interact with.
Correct me if I’m mistaken but I believe our job is to provide patients with the best level of care we can. Not the newest or most expensive but the best. Working out what’s best does require transparent collaboration and yes – listening to the opinions of others.
Could one describe the use of vecuronium a muscle relaxant which takes perhaps a minute or so longer than rocuronium to achieve muscle relaxation as a hazard? Not if one isn’t concerned about the rate of onset – for example a paediatric case where one wants muscle relaxation for the case but not necessarily the intubation.
However rapid muscle relaxation is not only beneficial for rapid sequence induction it is beneficial whenever we want muscle relaxation for airway management.
I doubt anyone would disagree that patients are generally easier to mask ventilate and intubate when paralysed.
At the time of induction patients are prone to desaturation. During this time if we prolong the time to successful airway maintenance we expose the patient to all sorts of unnecessary mischief – breath holding, increased airway trauma, hypoxia…..have I ever been to a morbidity and mortality meeting where vecuronium causing this issue because of its delayed onset is presented as such – well no. Does it happen? Undoubtedly – yet here I will be asked for the evidence as we enter the abyss of the wicked problem.
Am I going to raise an eyebrow at my colleagues using vecuronium?
🤔
Perhaps we should all think about wicked problems in healthcare a bit more.
We need all the help we can muster in trying to overcome these beasts – and in my opinion working together we can.
Let’s get our thinking caps on.

One Comment