Everyone who belongs in healthcare passionately wants the best for patients.
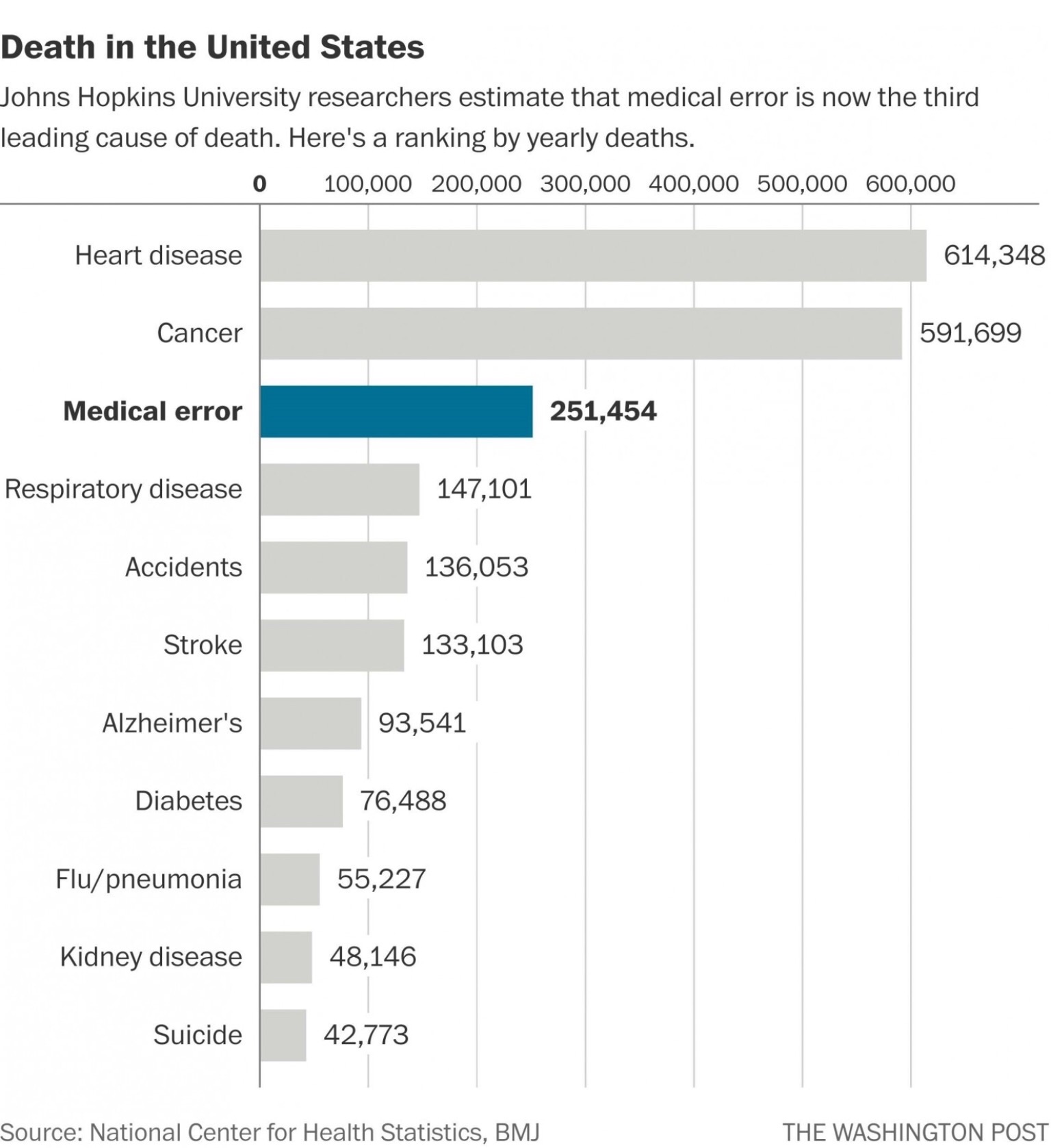
Medical error, however, has been reported as the third greatest cause of death.
We have tremendous opportunity to improve.
So what are the obstacles to patient safety?
Despite appearing simple, removing unnecessary hazards within healthcare frameworks is extremely difficult. This ongoing series of posts uses specific hazards to demonstrate the obstacles to patient safety.
We’ll persist to remove these hazards through generating support and interacting with healthcare bodies. Concurrently we aim to introduce frameworks which simplify the removal of other similar hazards.
Your qualities put you in a great position to demonstrate leadership. How can you help us all overcome the obstacles to patient safety?
Please click on each heading to read the posts in full:
Because what is our great fear in medicine? Hurting people. Not being good enough. And when we change a process for the better it inevitably implies that our PREVIOUS way of doing things was (at least relatively) harmful. To make a minor change for the better, we might have to accept we have been hurting people, maybe killing people (or putting them at risk of death) for years, even decades!
A disturbing (but very natural) ego-protective attitude occurs where staff reject innovations that make their carefully-honed skills less relevant. Senior clinicians may actively oppose or denigrate methods which are safer and/or more successful — not just for themselves but for their learners and the system as a whole too — in part because the innovation makes their own deft skill with the old tools less important.
In healthcare front line staff can’t access valuable information in their error databases. This lack of transparency leaves us flying blind. Without seeing our errors we can’t improve.
Psychologists launched a series of experiments resulting in one of the strongest and most replicable effects in social psychology. Is healthcare safety suffering the ‘Bystander Effect‘? Several factors contribute to this phenomenon.
‘When faced with a human error problem you may be tempted to ask ‘Why didn’t they watch out better? How could they not have noticed?’ You think you can solve your human error problem by telling people to be more careful, by reprimanding the miscreants, by issuing a new rule or procedure. They are all expressions of the ‘Bad Apple Theory’ where you believe your system is basically safe if it were not for those few unreliable people in it. This old view of human error is increasingly outdated and will lead you nowhere.’ – Sidney Dekker.
‘The Gap’ exists between work as perceived by managers and work as performed by front line staff. This gap is endemic to top down safety approaches.
‘While most of us assume that “errors = accidents”, aviation knows that “errors – safeguards = accidents”. By obsessing over error reduction (via root-cause analysis), we miss opportunities to increase safeguards. – Nick Argall.
Our hospitals are increasingly complex and humans err. We need to understand the healthcare safety problem is not bad people. Adverse events will continue to occur if we don’t act wisely.
Adverse events, by their nature, are dispersed in time and place. Given we’ve numerous different error reporting systems, which don’t inter-communicate, the effect of dispersion is compounded. Adverse events, as a result, are presented as ‘one off events’.
10. Alerts & Other Less Effective Interventions
It’s counter-intuitive that an alert designed to improve safety may actually be detrimental to patient care. Unfortunately alerts on their own may absolve governing bodies from ensuring more effective interventions.
Front line work environments are full of unnecessary distractions detracting focus from the task at hand. They come in many forms from a noisy vacuum cleaner disrupting a patient consult, to a poorly designed electronic medical recording system. Removing distractions will lead to improved patient outcomes. Top down healthcare frameworks, however, impair our ability to do this.
12. Bullying, Threats & Intimidation
If patient safety is to improve healthcare will need to transition from its historical top down approach to one where the voices of front line staff are truly heard. This may require thousands of small steps taken by numerous staff deciding to demonstrate leadership. Perhaps the most primitive but effective way of stifling change is through bullying, threats and intimidation. Be prepared.
Uttered by those in authority to maintain the status quo it can stop a patient safety intervention in its tracks. However doing the best possible for every patient is priceless.
We are avid supporters of evidence based practice, however we recognise how it can be used inappropriately as a tool to stifle change. Ultimately this is of detriment to our patients.
Command Structures within healthcare often lead to extremely weak safety interventions – those at the top may have poor understanding of front line conditions.
Competition can help drive improvement up to a point, after which it may perpetuate unnecessary harm.
17. Key Performance Indicators
‘Key Performance Indicators’ impair staff morale, add unnecessary pressure to achieve an arbitrary target and are ultimately detrimental to patient care. Perhaps instead we should measure patient outcomes and the satisfaction of front line staff. Interventions collaboratively developed on the front line could be trialled and their impact on these measures assessed.
18. ‘Never Events’ or ‘Always Conditions’?
This brilliant post by Steve Shorrock discusses why the label ‘never events’ is detrimental to improvement given they always happen.
19. Reputation – a Wicked Problem
How much does reputation affect patient safety?
20. Social Conformity & Groupthink
If patient safety is to improve we’ll need to think critically about our accepted norms.
The Bleeding Edge documentary highlights how greed and corruption in the medical device industry causes significant patient morbidity. This may represent the tip of the iceberg.
Your qualities put you in a great position to demonstrate leadership. How can you help us all overcome the obstacles to patient safety?
We’re interested and will all benefit tremendously from your insights, feedback and support.
