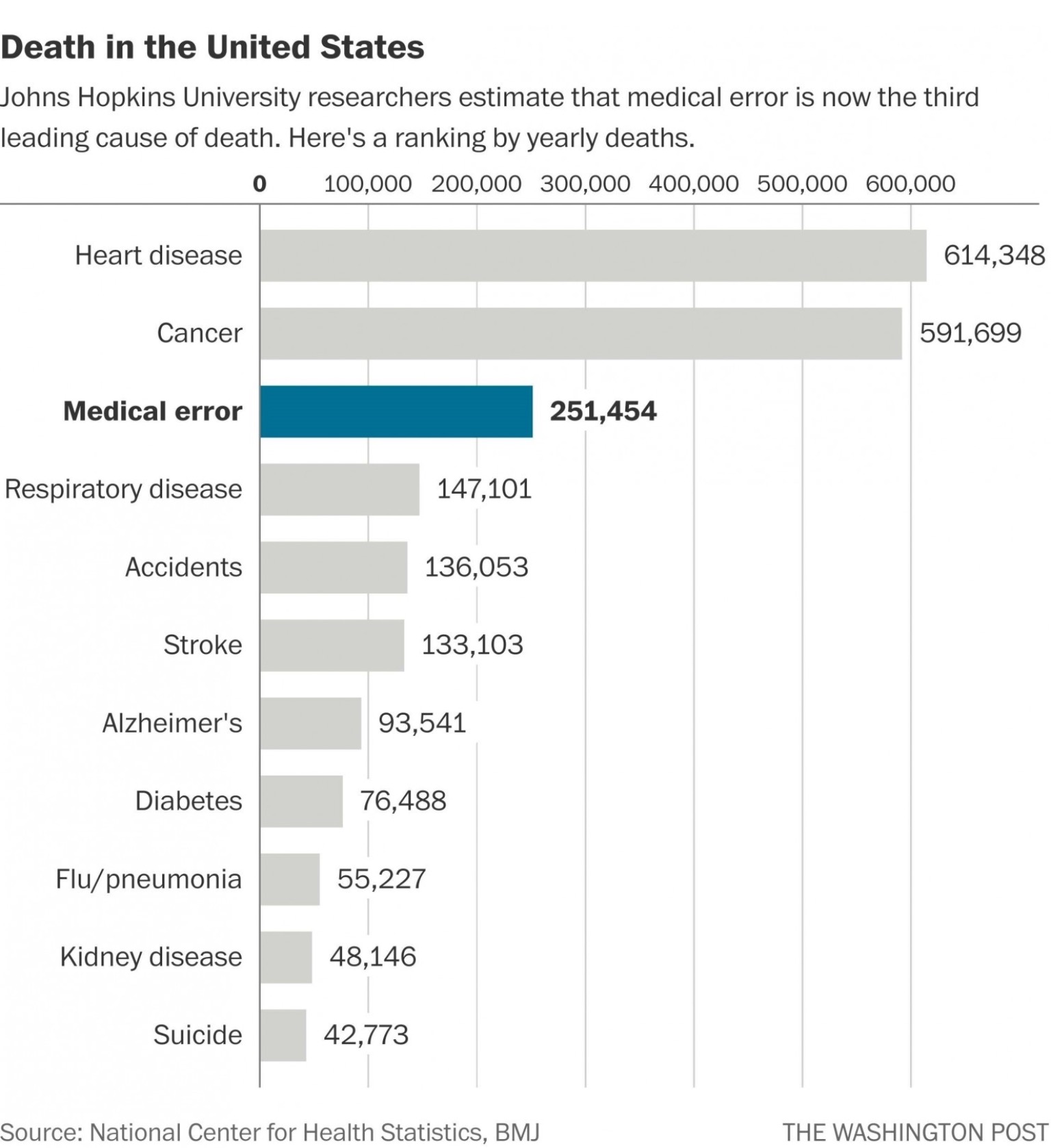
Everyone I’ve ever met in healthcare wants the best for patients yet medical error has been reported as the third greatest cause of death.
I’ve spent years focussing on patient safety projects and learnt how current healthcare culture often stifles improvement. All the while I’ve been desperately searching for a way forward.
In healthcare we’d all benefit from better understanding of human factors and system safety.
Think back to an era when infection control came to being and the struggle Dr Semmelweis had trying to get staff to wash their hands. There are many obstacles to delivering patient safety improvements. Perhaps one is that, within a healthcare command hierarchy, those who are last to accept new practice often have the greatest influence.
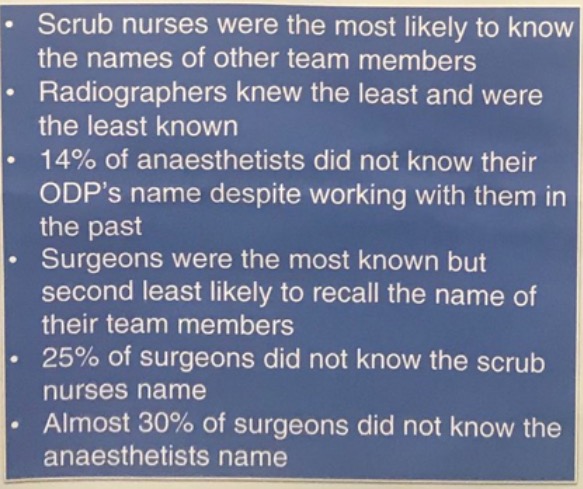
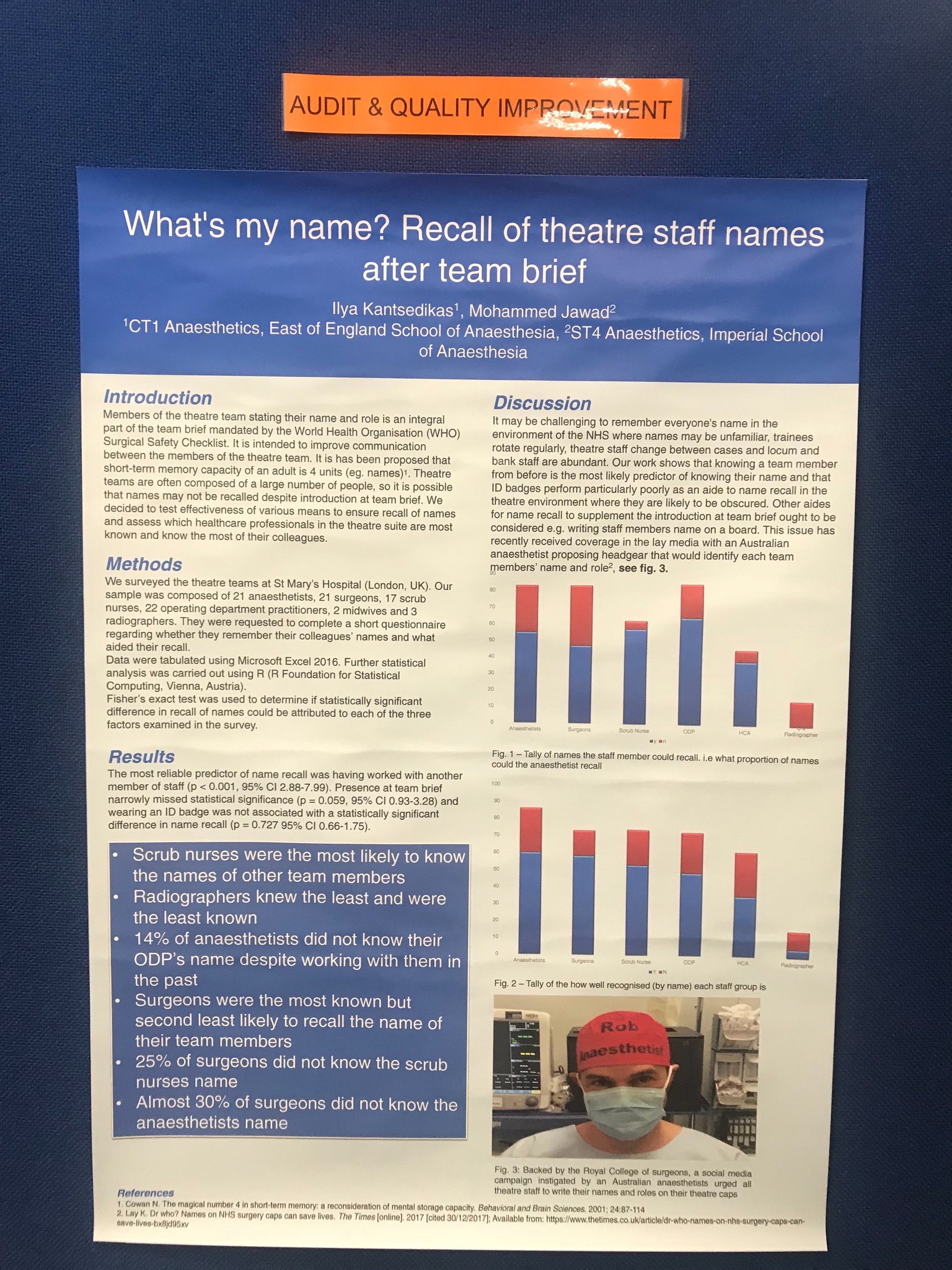
When theatre staff truly understand human factors, human limitation (we forget people’s names) named theatre caps will be readily accepted.
The #TheatreCapChallenge is a win – win situation for patient safety.
The only thing from stopping it happening is us.
Either we adopt it – introducing an obvious and effective patient safety intervention
Or we don’t – demonstrating how structures in healthcare are resistant to change.
There’s no doubt many other staff had the named hats idea – I read comments on social media to this effect. Perhaps the fantastic support from friends, family and an invaluable quality and safety fellow – Dr Rhys Thomas allowed me to pursue this given the resistance, ridicule and immense kickback imposed in driving any change.
Yet stamina and amazing support alone is never enough.
What caused the theatre cap idea to tip was something command structures may never possess – the ability to truly listen to and support front line staff to develop effective solutions. In this case the brilliant idea of a student midwife on the other side of the world – Alison Brindle and her #TheatreCapChallenge.
Healthcare needs to embrace a transparent networked team of teams where front line staff work together with patients, human factors experts, manufacturers and others – their projects, facilitated by those in charge, allowed to flourish.
These are just some of the projects we’re working on through the Patient Safe Network (psnetwork.org). We’re excited that as healthcare frameworks and culture changes there’ll be hundreds more patient safety projects driven to fruition:
Bankstown Hospital was struck with tragedy last year – babies given nitrous oxide instead of oxygen. Gas pipeline errors, like the one which caused this recur, with persistent frequency. The response to the Bankstown tragedy is almost identical to one in 1973 where 23 people died – blame and rewrite a policy. This will do little to prevent the same adverse event. Use of oxygen analysers at all areas of airway management will – however it’s yet to be mentioned by those in authority reviewing the case.
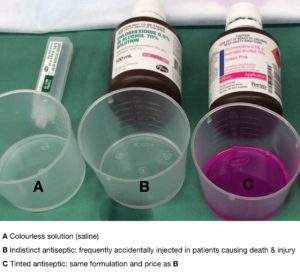 Indistinct Chlorhexidine – Indistinct chlorhexidine has been accidentally mistaken for colourless solutions and injected into patients on numerous occasions causing death and morbidity. Vividly coloured alternatives exist at no extra cost. Over 500 front line staff have signed the petition to ban pourable indistinct chlorhexidine – perhaps a sorry reflection of healthcare that we petition to remove an obvious unnecessary hazard.
Indistinct Chlorhexidine – Indistinct chlorhexidine has been accidentally mistaken for colourless solutions and injected into patients on numerous occasions causing death and morbidity. Vividly coloured alternatives exist at no extra cost. Over 500 front line staff have signed the petition to ban pourable indistinct chlorhexidine – perhaps a sorry reflection of healthcare that we petition to remove an obvious unnecessary hazard.
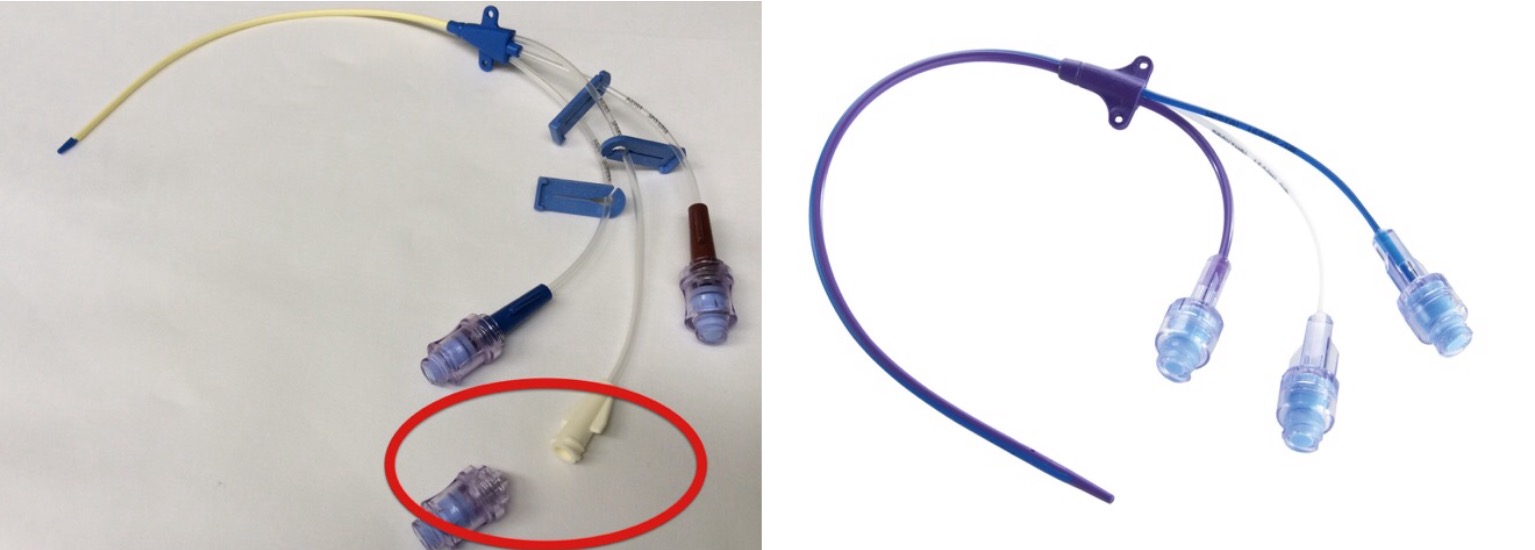
All Central Venous Lines currently inserted into patients throughout Australia and much of the rest of the world open to air yet we don’t need them to. Hundreds of patients die every year because these lines are accidentally left open to air – air is then sucked into them causing air emboli, cardiac arrest and death. Please watch this video to learn more (see here). Central lines with bonded caps which can’t be accidentally left open to air are already used without issue and at no extra cost. After watching the video please consider why these lines aren’t already standard – the command structure of healthcare creates a culture which stifles change.
The most effective patient safety interventions focus on the systems and equipment front line staff interact with however front line staff have little control over these.
When you follow current command frameworks all the way to the top, to the groups charged with ensuring we’re working with the safest devices and medication you’ll discover these groups – the TGA, MHRA, FDA – don’t support the front line. They support, and are almost completely financed by, the companies whose devices they’re supposed to govern. Little wonder we can’t get rid of indistinct chlorhexidine. For a great insight into the level of corruption in the US$400billion medical device industry please watch ‘The Bleeding Edge’.
Medicines and devices are heavily marketed and driven in to healthcare institutions. Where they’re identified as hazards to patient care front line staff need the power to remove them.
We need an army of people, who understand human factors, collaborating as a networked team of teams, with the courage to drive projects for patient safety. Thanks to Alison Brindle and her #TheatreCapChallenge, within theatre, this army’s become easier to identify.
Thank you Alison Brindle – this is more than a human factors solution, it’s a statement we make to help save thousands of lives:

Please click on any of the links in red to read more.
There’s an increasing number of suppliers of name & role theatre caps (see here) – please let us know if you hear of any more and we will add to the list.
For healthcare staff working outside theatre #hellomynameis badges can be purchased online (click here).
Thank you for your support.
2 Comments