Everyone wants patient safety to improve. Together we can make it happen…..
Front line healthcare work environments are increasingly complex with new drugs, equipment and a constantly changing workforce. Individual staff may work across several different insitutions, at times being brought together rapidly (for example during cardiac arrests) forming teams working with individuals they may never have met before.
The greater the complexity the more likely mistakes will be made.
Adverse events have been reported into hierarchical command structures – those at the top who receive the bulk of the information often don’t work on the front line. Proposed interventions traditionally focus back on front line individuals through education frameworks, policy writing and alerts.
These serve in themselves to further increase the complexity of front line work environments.
Cultural peculiarities in healthcare have perpetuated this approach. Doctors are academic achievers nurtured in competitive environments. They succeed through competition to achieve their positions in the hierarchy. They thrive on complexity and believe an ability to deal with complexity stands them above their peers. Removing complexity can take away a competitive edge the knowledge about it offers.
Governing bodies established to improve safety may be concerned about their own reputations and the legal implications of removing identified hazards from the front line – they may fear litigation from the drug/medical device companies (poorly distinguishable chlorhexidine still exists on the front line – governing bodies instead of removing it have used alerts and policies to address the issue – see here).
Attacking complexity with more complexity sends us in the wrong direction. While everyone wants patient safety to improve we’ve followed a pathway which has taken us away from it.
We are going in the wrong direction:

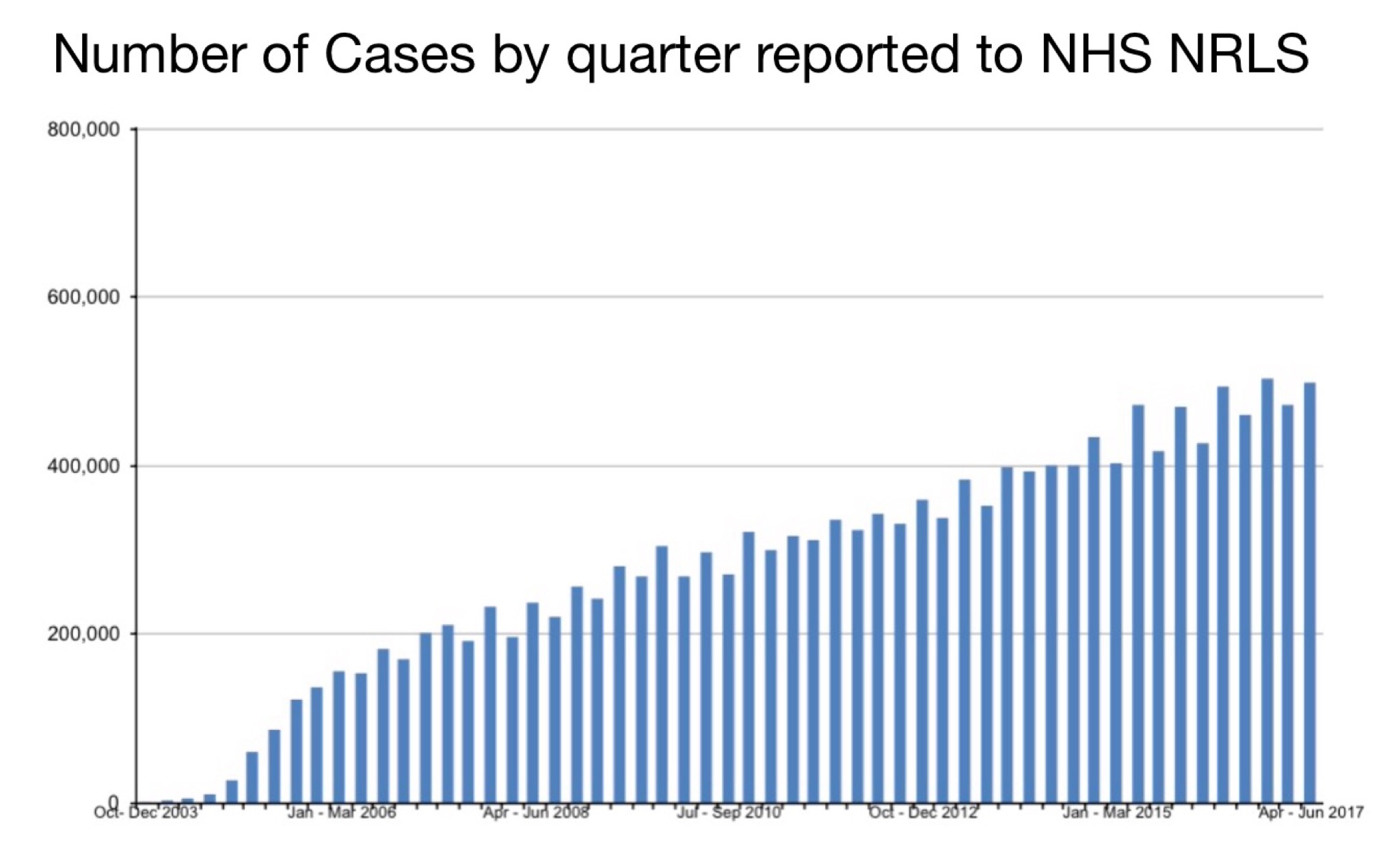
How bad have things got?
Its hard to say as our error reporting systems lack transparency and they don’t communicate with one another (see here). A recent estimate published in the British Medical Journal put medical error as the third greatest cause of death:

Why don’t front line staff do something about it?
Many do try however command structures reinforce the status quo. It’s extremely easy for individual voices to be put down. Despite this many have persevered beyond the abuse, bullying and intimidation that may be applied to quell their voices only to become isolated as ‘whistleblowers’ – many left without prospect of employment.
Has anything managed to get through?
Recently the #TheatreCapChallenge (see here) has seen widespread adoption by many front line staff. The initiative has had little if any support from governing bodies some searching for ways to suppress what is an obvious improvement for patient safety. There are many tools which can be applied (show me the evidence, infection control). The #TheatreCapChallenge has persisted regardless and where it has been resisted this has served to expose how command structures can suppress change and improvement.
There are hundreds, perhaps thousands of similar design changes which need to take place for patient safety to improve.
How can we introduce better designed equipment and systems into healthcare?
Front line staff collaborating with human factors experts (Shorrock to create list of HF experts) and other relevant parties can transparently grade the equipment and systems they interact with providing a score similar to the ‘energy efficiency rating score’ provided for electrical appliances:

The scoring system can be inclusive and encouraging e.g. 5 points for most user friendly piece of equipment, 1 point for least user friendly, 0 points if no information provided regarding that piece of equipment.
This independent scoring generated in a way similar to ‘Which’ or ‘Choice’ magazine. There will be some issues that present a greater latent safety threat than others and scoring should be weighted to reflect this.
Information can be obtained about what equipment and systems hospitals currently have in place and how ‘usable’ it is. This information can be tallied and hospitals provided with a score to rank how usable their sytems & equipment are overall. Publishing this data will then help drive both hospitals and device manufacturers to change and improve.
Are hospitals willing to be included in ranking systems?
The NHS already provides league tables based on performance criteria as assessed by front line staff (see here).
NSW has allowed assessments from junior staff and subsequent ranking (see here).
How can groups of independent front line staff, human factors experts and others collaborate to generate decisions about equipment/system usability?
BaseCamp and similar software allows efficient rapid collaboration. Transparency with discussions can allow crowd sourcing for additional information to be ascertained.
What is to stop this process being corrupted?
Complete transparency in decision making and discussions on system & equipment usability. Anyone can access this information and provide their opinions.
How can information about the usability of different equipment & systems be easily provided for others to see?
Brief 2 minute videos succinctly discussing the implications of the usability of specific equipment/systems can be created. (Ant) These can link to further information on the topic and how to communicate with the specific (BaseCamp) group.
The videos and links can also provide free R&D suggestions for future system/equipment improvements.
How can we obtain information about what systems/equipment hospitals are already using?
Make a game of it – the simpler and more enjoyable we make it for front line staff to provide this information the more likely they will be to do it. (Whiteboard.is)
We all carry extremely powerful smart phones in our pockets – these provide the hardware for out ‘point of care’ software platform. Making a game which is simple, enjoyable and that people want to interact with will allow us to capture the data we seek. (Read more about gamification here).
Are front line staff willing to provide information about the systems and equipment their hospital uses?
Yes – a recent initiative to standardise the ‘Crash Call Number’ in Australian hospitals used crowd sourcing through social media to identify a myriad of different phone numbers at different hospitals (see here). Through initially focussing on equipment and systems which staff have no emotional attachment to we can gradually gain their confidence in providing information.
What might cause front line staff to hesitate about providing this information?
Staff may be concerned about how it might impact negatively on their careers. This is not something they have done before – it’s steps away from the status quo. We can help overcome this through
– anonymity – use of ‘avatars’ in the PatientSafe Game providing staff or others revealing information with anonymity
– reviewing ‘Code of Conduct’ and ‘Contract Agreements’ and providing information on how these impact in revealing information (Rob & Rhys).
As well as creating league tables what else can be done with the information?
Emails can be sent directly to heads & other relevant staff of a particular hospitals highlighting the specific system and equipment improvements they can make. (Brad obtain email addresses)
Given the process of forwarding this information via emails etc is not a commercial activity then it should not be constituted as spam in accordance with the spam act (see here).
It would be ideal to create a pilot and then assess how this system might work across a series of hospitals (consider Ramsay Health – Jo & Silas)
I’ve personally carried out a very crude version of The PatientSafe Game at my hospitals. I’ve fed information about how each hospital may improve back to relevant staff. They’ve welcomed it and some have started to implement change based on this.
A list of equipment/system projects (subgames) with links and lots of other relevant information – (see here).
Potential issues/questions regarding the development of this system:
– How will the software appear – as an App, rating site like (trip advisor), both, something else?
– Will people be able to post into it completely anonymously or will they need to provide some secure details about themselves? If details are provided then how do we best maintain their security?
– How best to prevent spamming from drug/device companies or others?
– How best to agree on weighting scores of subgames (?collaborative transparent approach lead by senior human factors expert & front line staff members specialising in that affected area).
– How best to prepare for inevitable push back from hospitals? (Endorsement by influential groups and individuals in healthcare)








