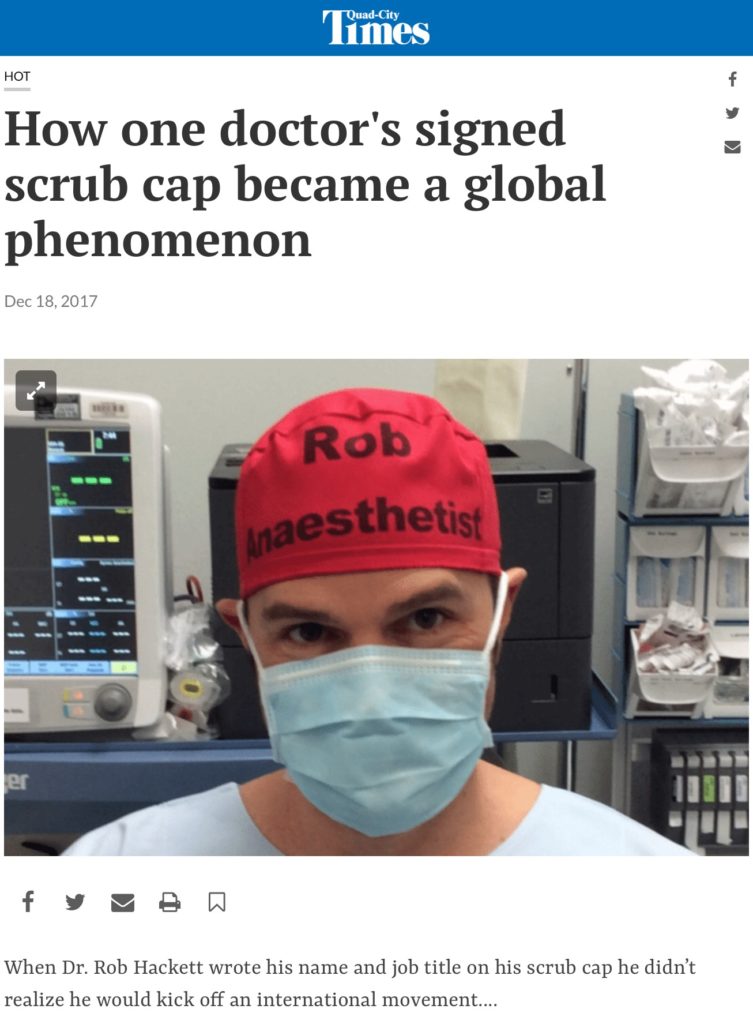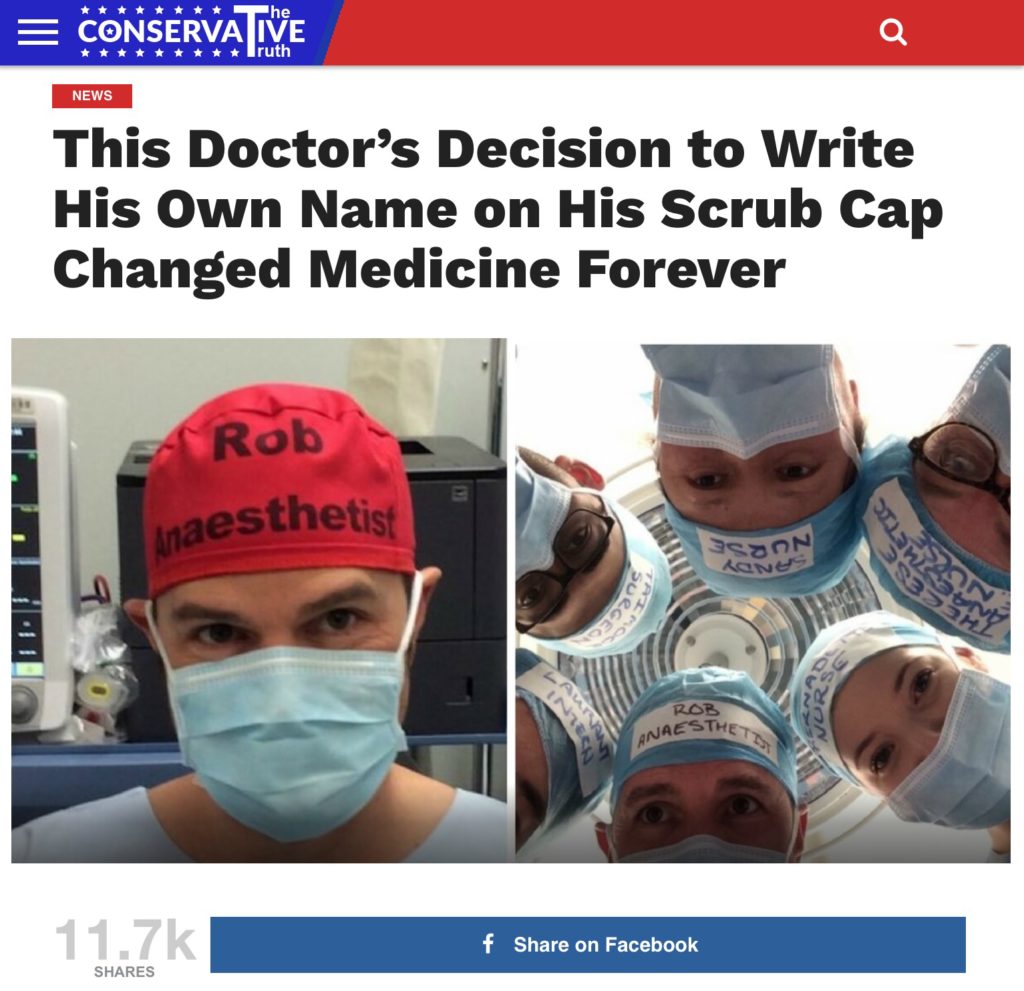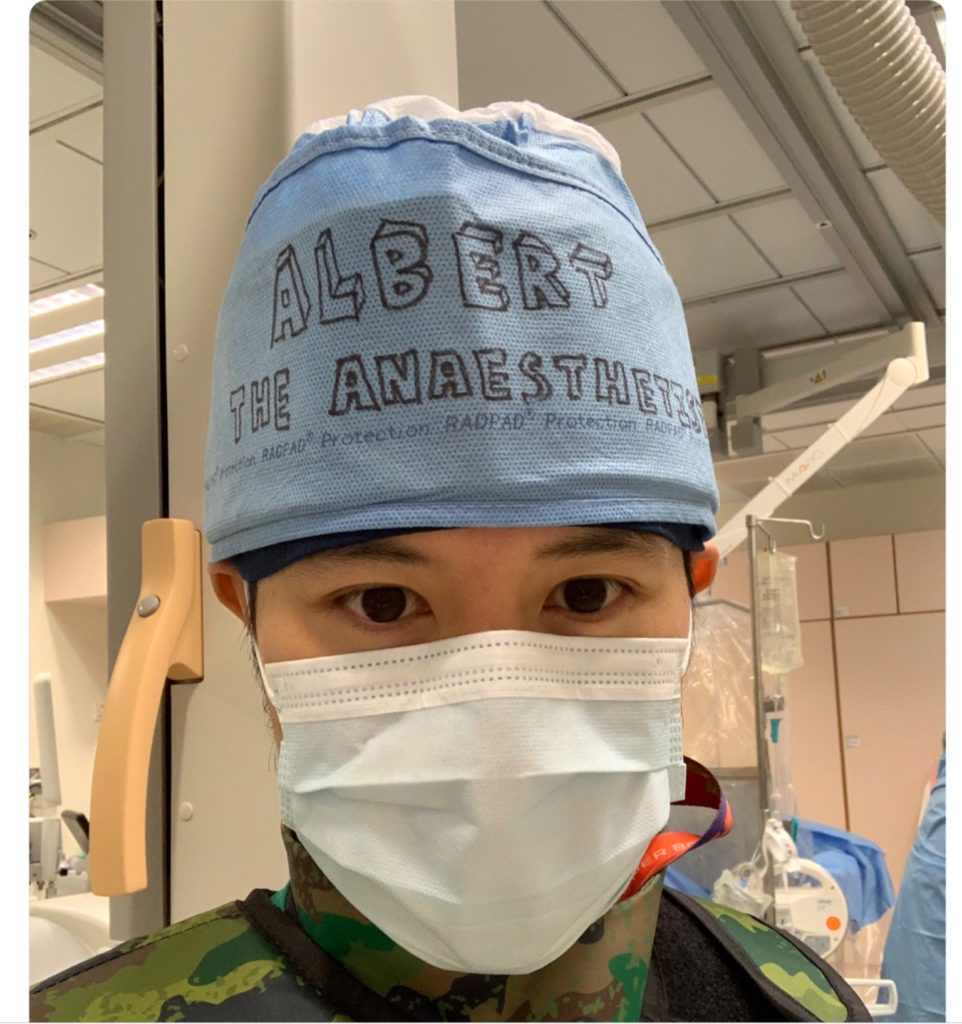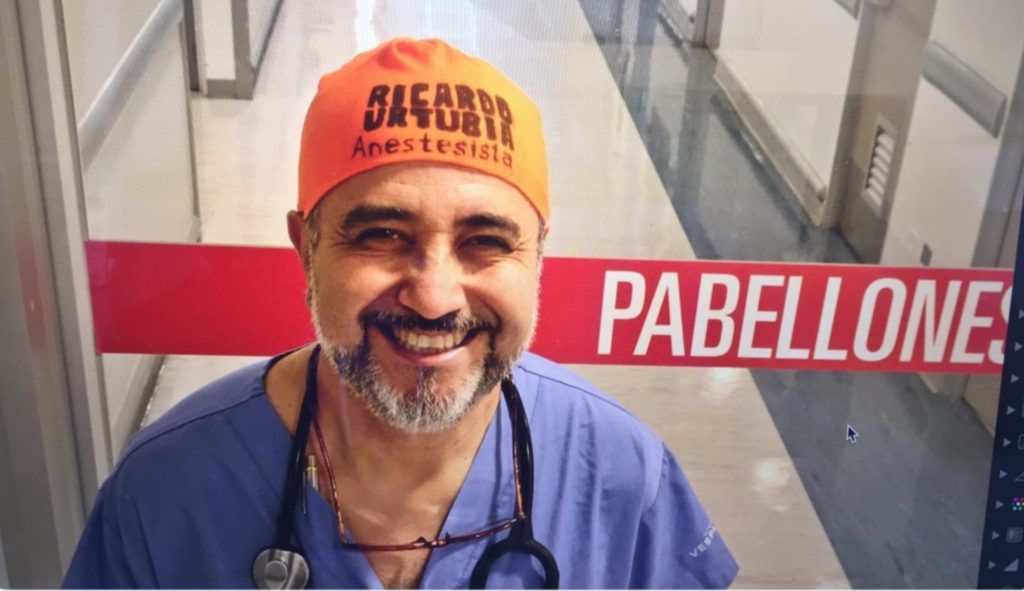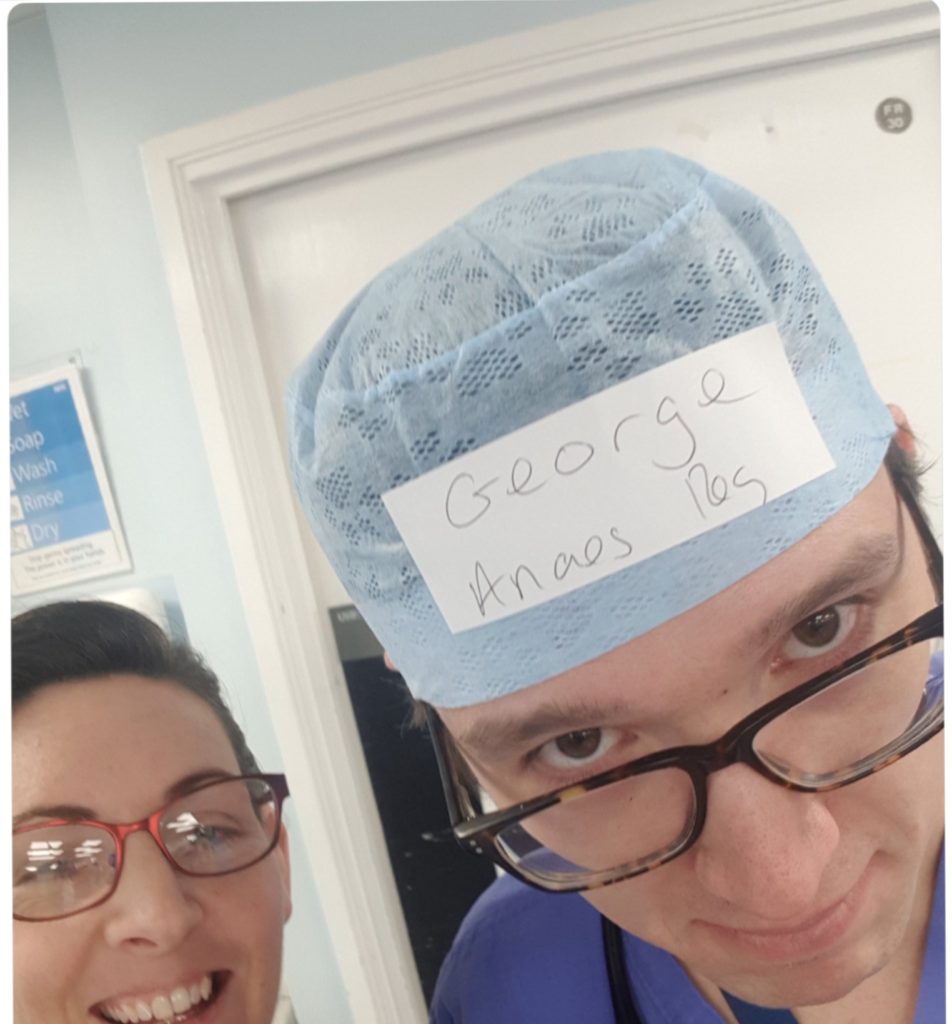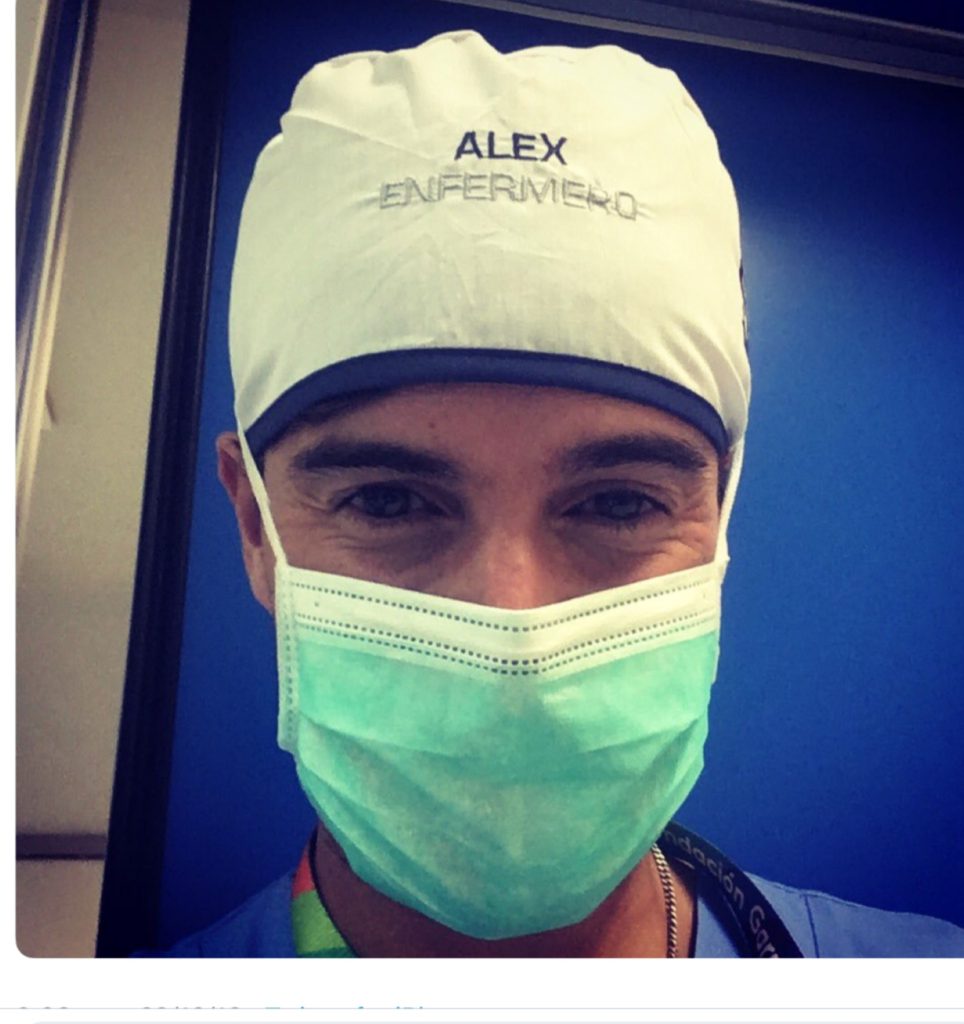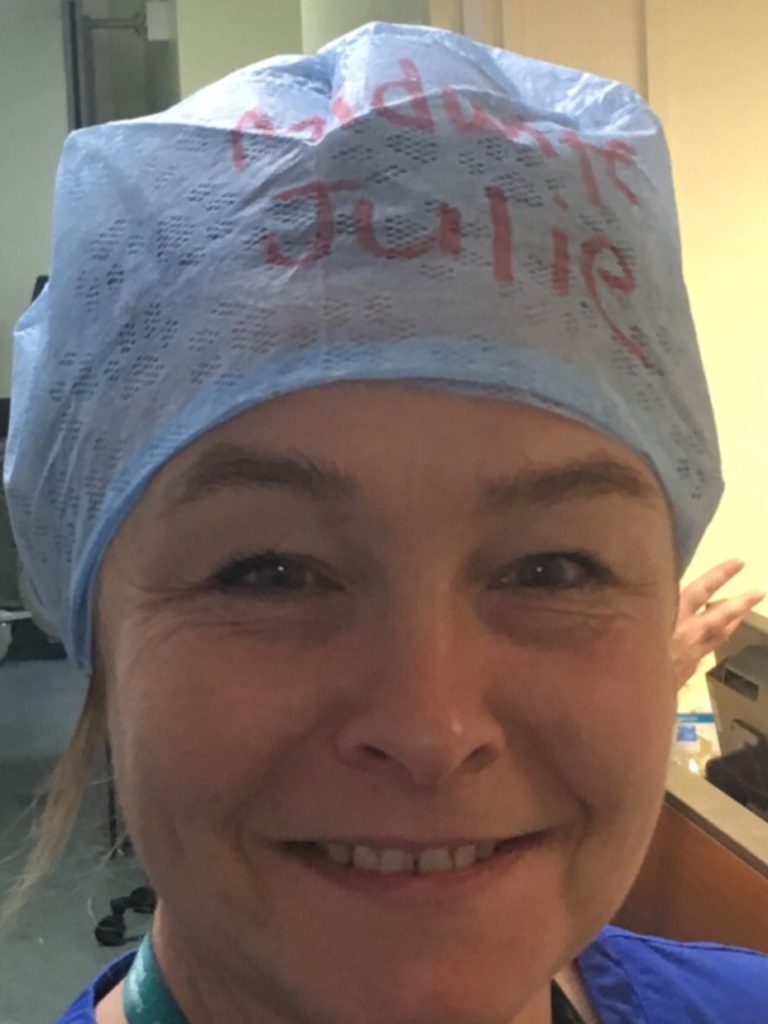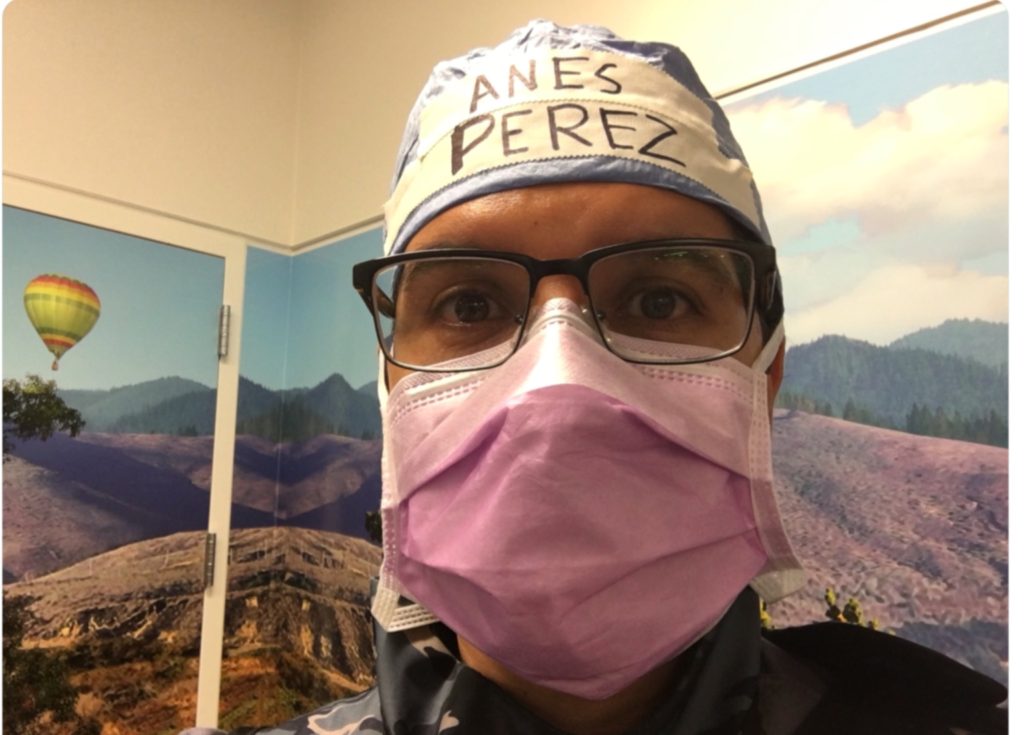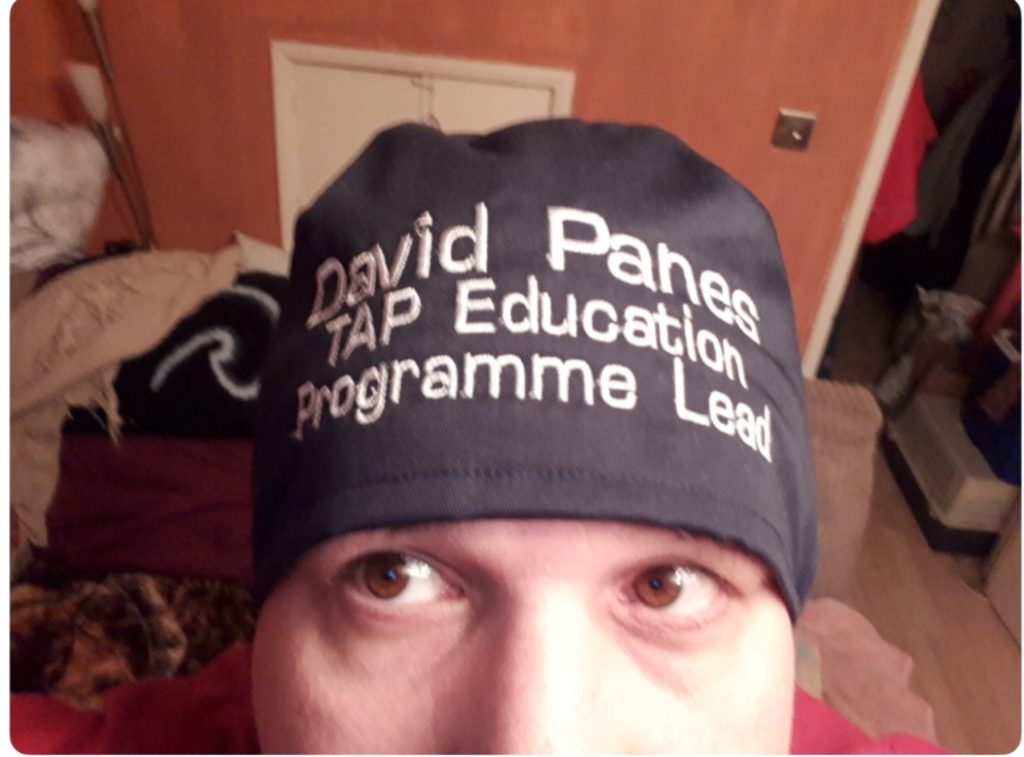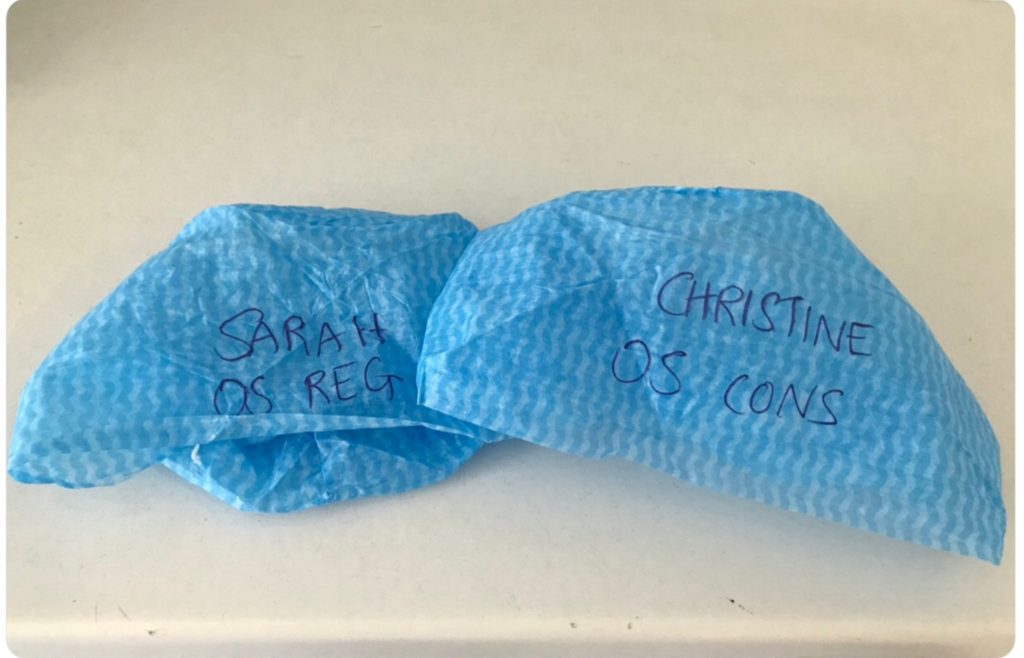
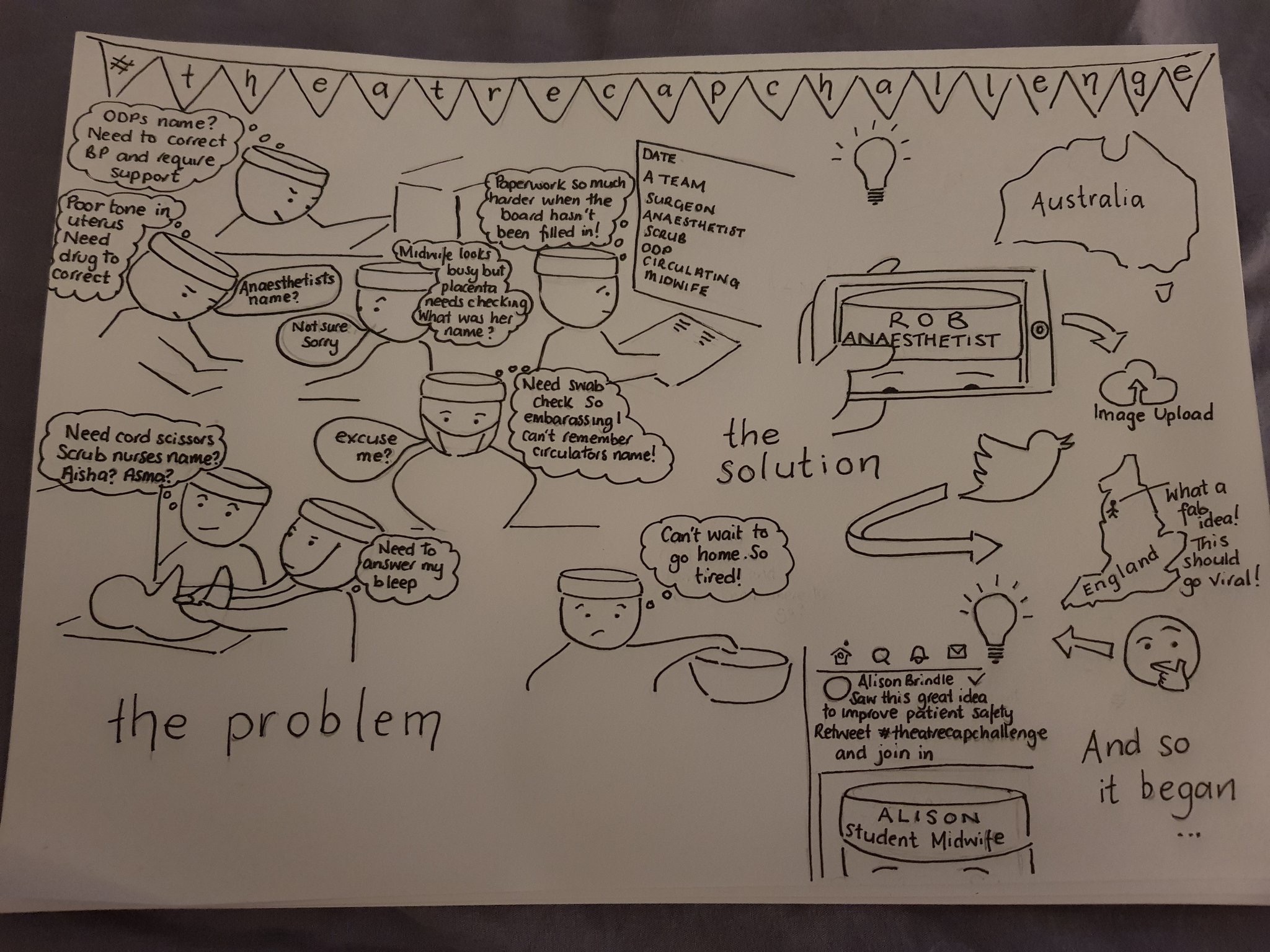
Thank you to all those who have already and continue to provide data on this initiative through international collaboration. There’s an increasing number of personalised theatre caps worldwide (see here) – so what’s all the fuss about.
We’ve put some quick links together at the start of this post:
General communication errors
- 70% of adverse events related to communication errors
- Communication failures in 30% of theatre team exchanges, 1/3 of which lead to inefficiency and increased tension
Staff misidentification
- Numerous cases of adversity including death from wrong blood transfusion.
- 4 out of 5 female doctors report being misidentified
Increased staff engagement through knowing names
- Cocktail party effect
- Hearing one’s own name has unique brain functioning activation
- A person’s name, to that person, is the sweetest and most important sound in any language.
Staff poor at introductions
- How good are doctors at introducing themselves?
- Poor compliance with name and role introduction part of Surgical safety checklist
- Only a small fraction of patients could successfully identify at least 1 physician or trainee on their inpatient team in charge of their hospital care.
Difficulty for staff to recall names
- Even when not distracted humans only remember 30% of names after first introduction then we readily forget them
- Social stress-induced cortisol elevation acutely impairs social memory in humans.
- Humans poor at remembering names good at remembering faces
- Surgeons only knew 44% of names
- Even after time out introductions performed 25% of surgeons did not know the scrub nurses name and 30% of surgeons did not know the anaesthetists name
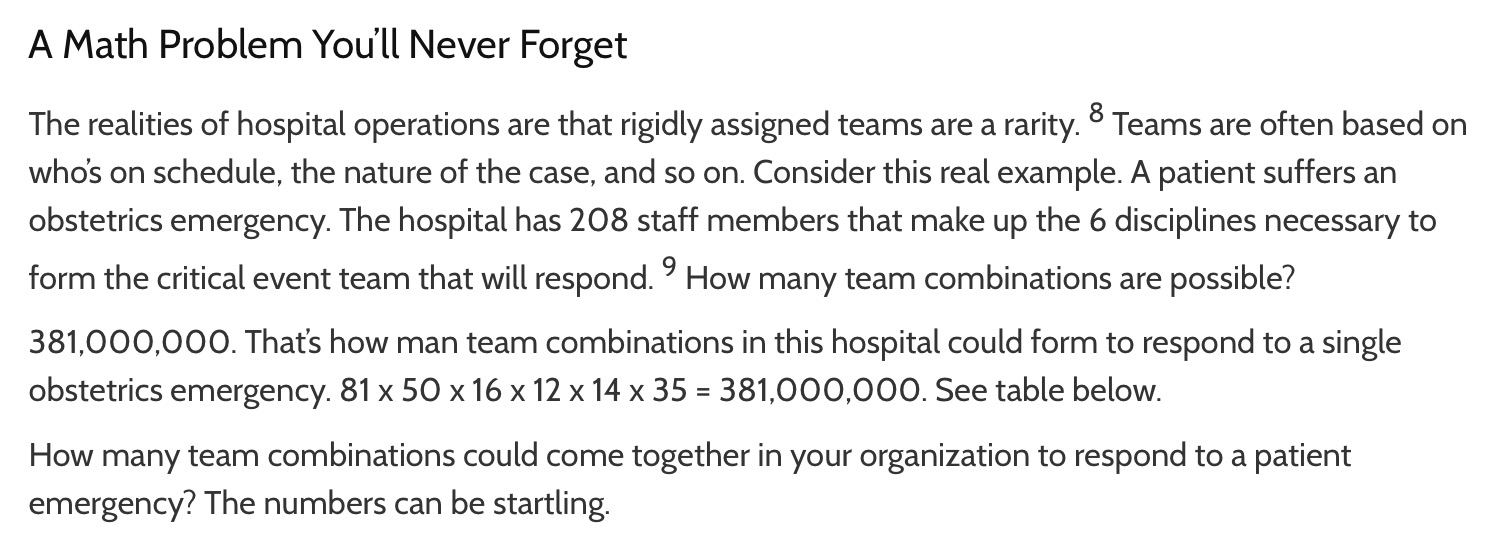
- Number of different combinations of team coming together to manage an obstetric emergency 381 million
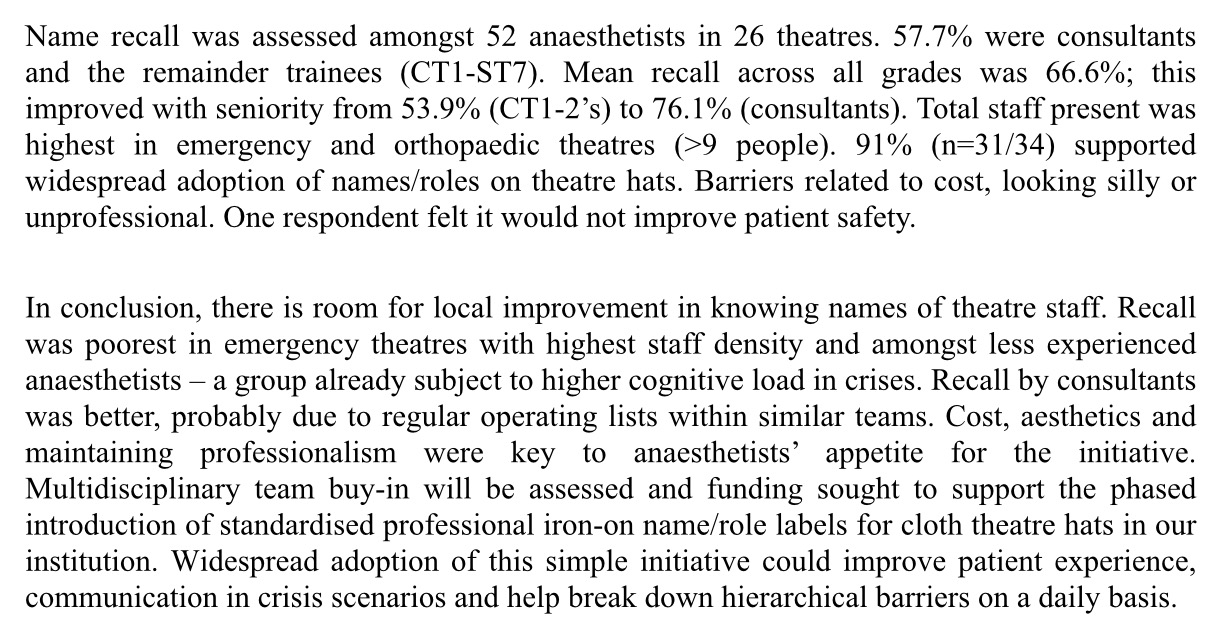
- BJA – name recall worst in Emergency theatres
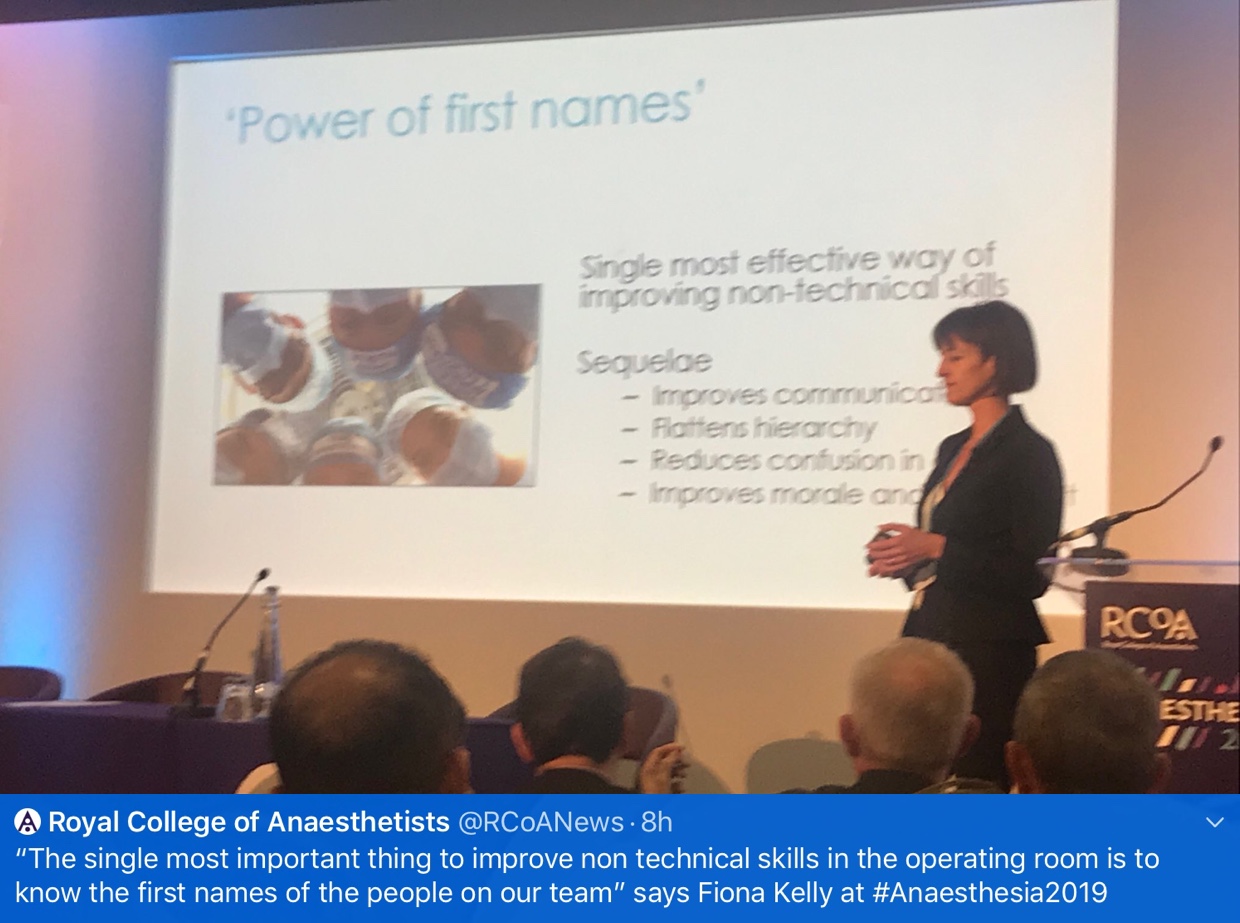
Studies indicating benefit in using names for communication
Supportive policy
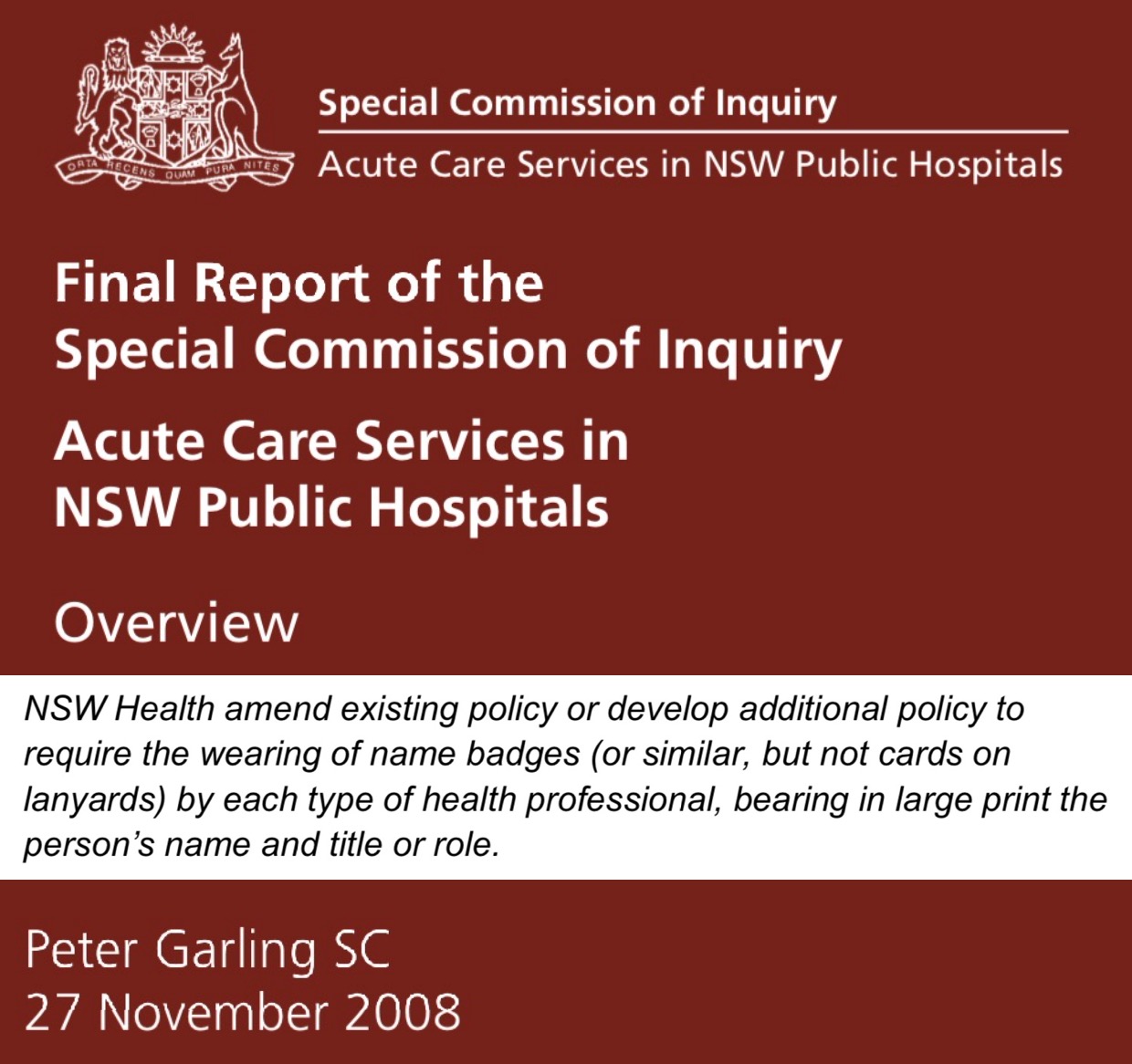
- Garling Enquiry 2008 – all healthcare staff should wear badges or similar bearing in large print the person’s name and title or role.
- NSW Policy 2008 – Nurse in charge will ensure all staff are easily identifiable
Why use a theatre cap and not just use a badge, lanyard, whiteboard?
Survey data
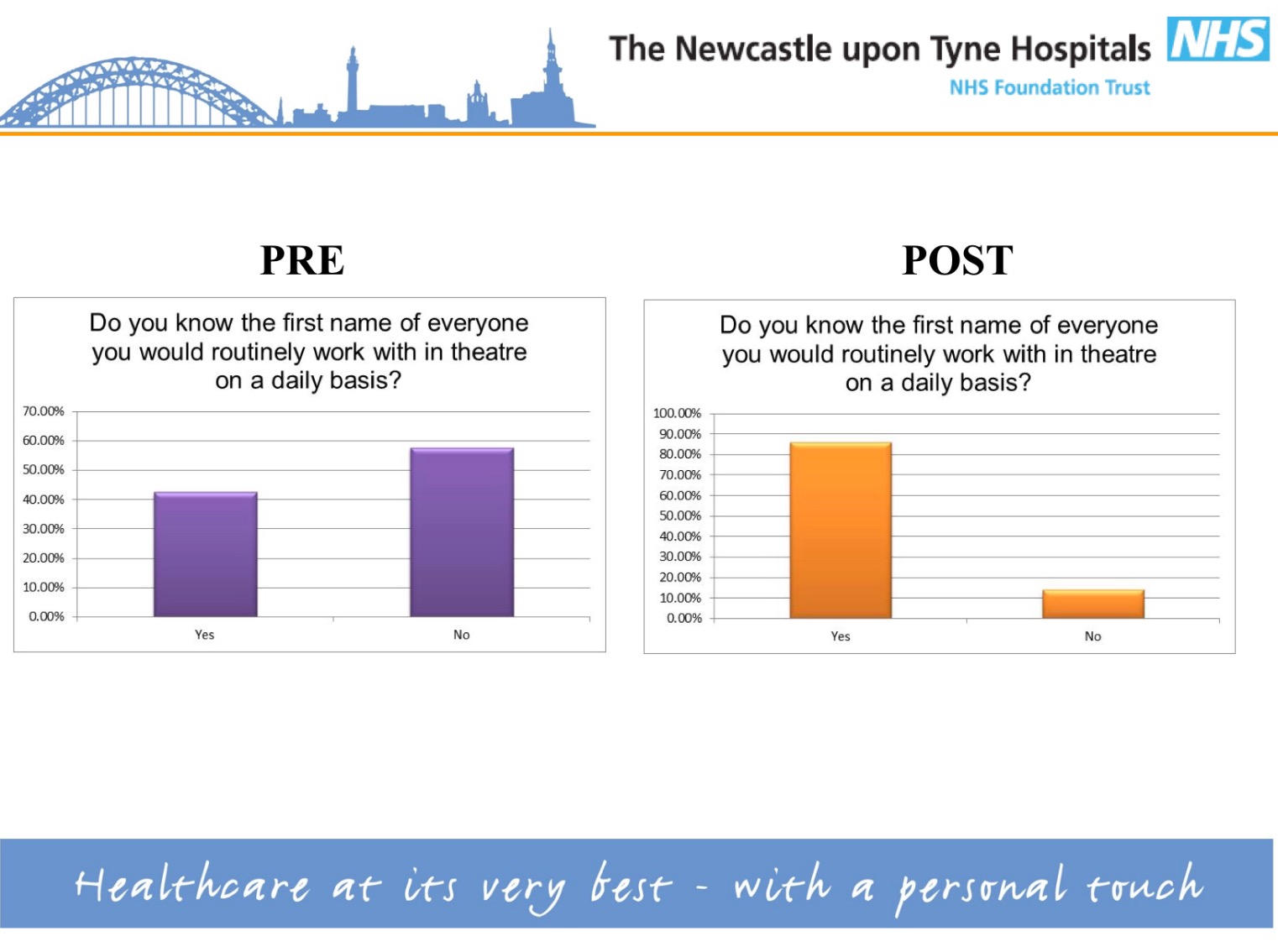
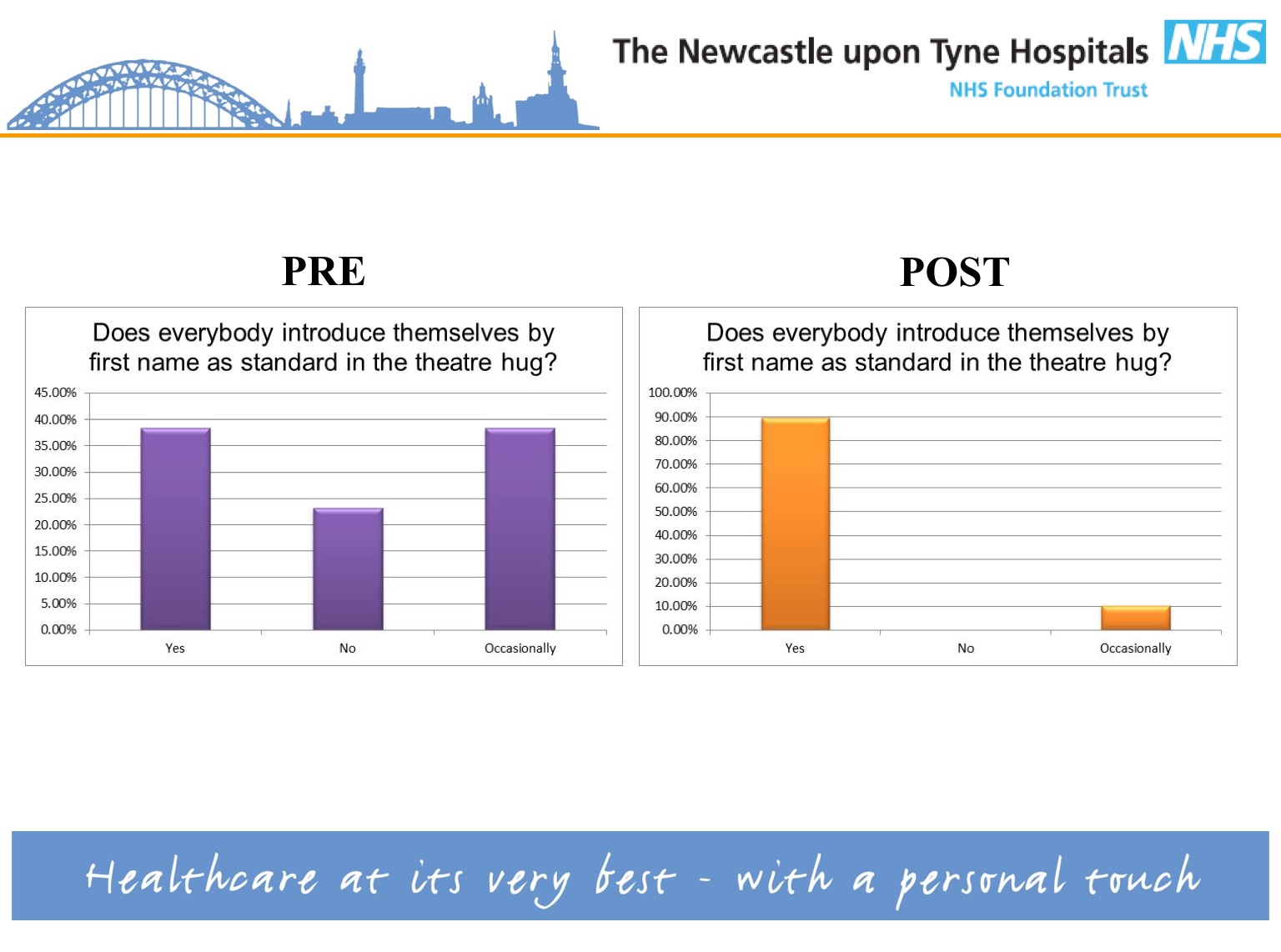
- #TheatreCapChallenge led to increased name & role introductions from 38 to 90%, increased name recall from 42 to 85% and increased propensity to speak up from 45 to 85%.
- Overwhelming support from staff – Imperial College London
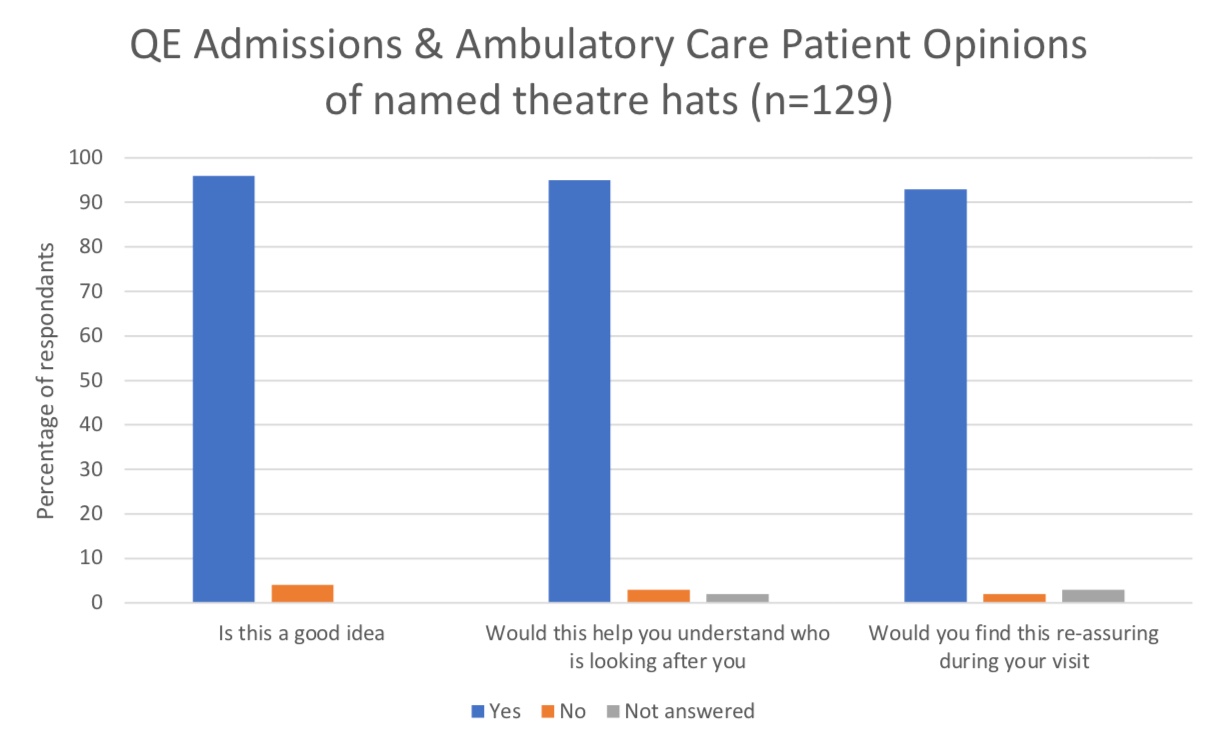
- Overwhelming support from patients – Queen Elizabeth Hospital
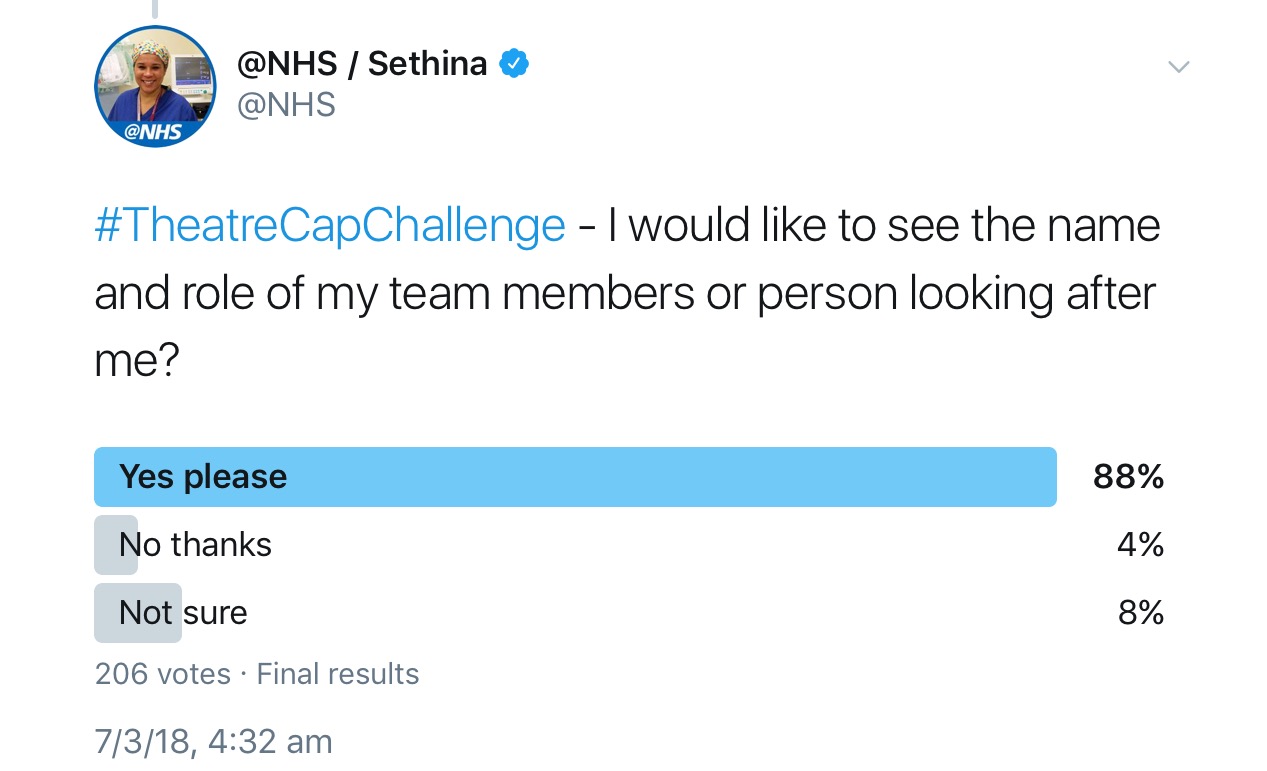
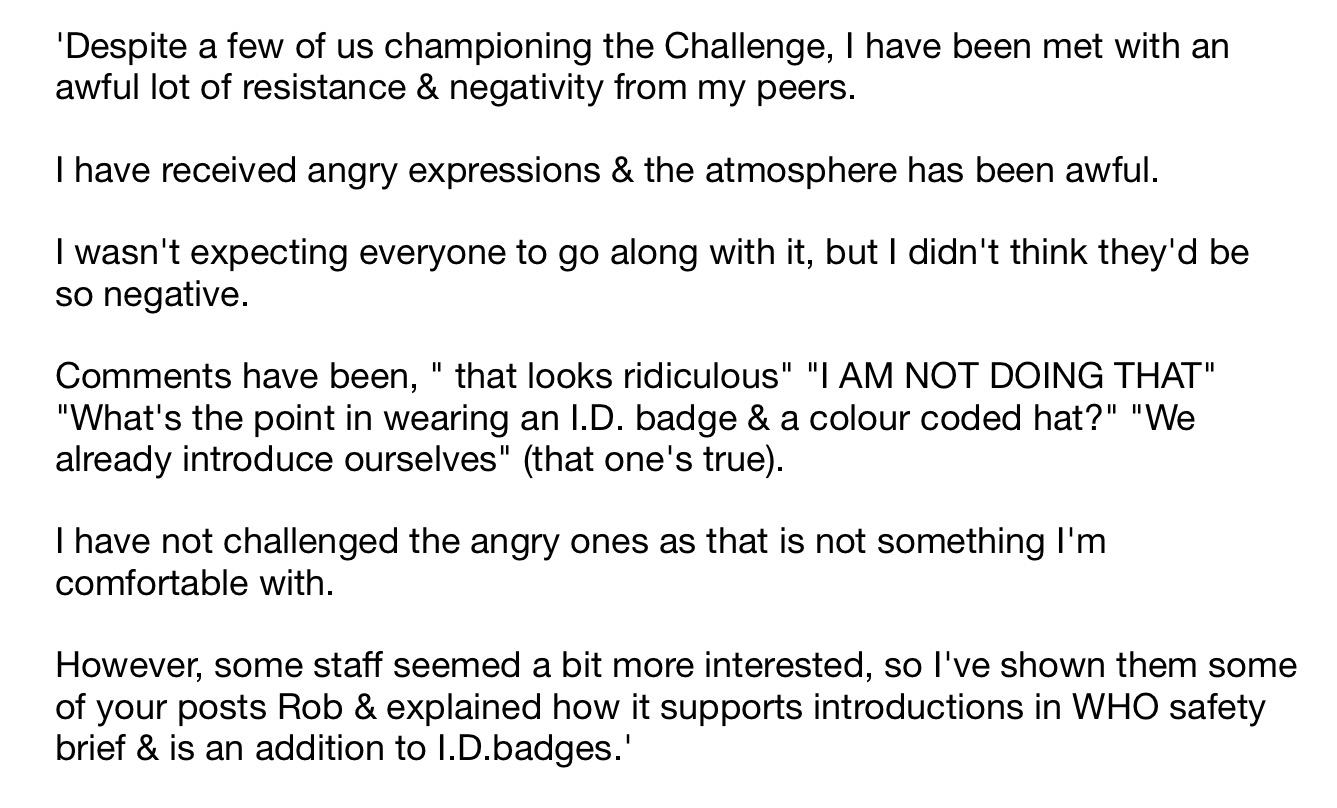
- 86.5% support on social media survey
- 88% support on twitter poll
- 80% agreed that names and roles on hats either did or could improve communication – Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust
Qualitative data suggests introductions help with identification of roles, improve morale and team performance (and see here). However emerging data indicate these introductions have little impact on name recall amongst staff.

Simulation data
- Stanford University simulation – The response during this simulation was the most efficient and effective of any simulation we had ever run. In particular, we found communicating directly by first names enhanced the participant’s ability to have closed-loop communication.’
- Awaiting publication of data from Marlies Schivjen – Professor of Surgery, Amsterdam
- Grant from ACI – working group progressing on obtaining outline & data
Support from associations
- Endorsed by Australian Society of Anaesthetists
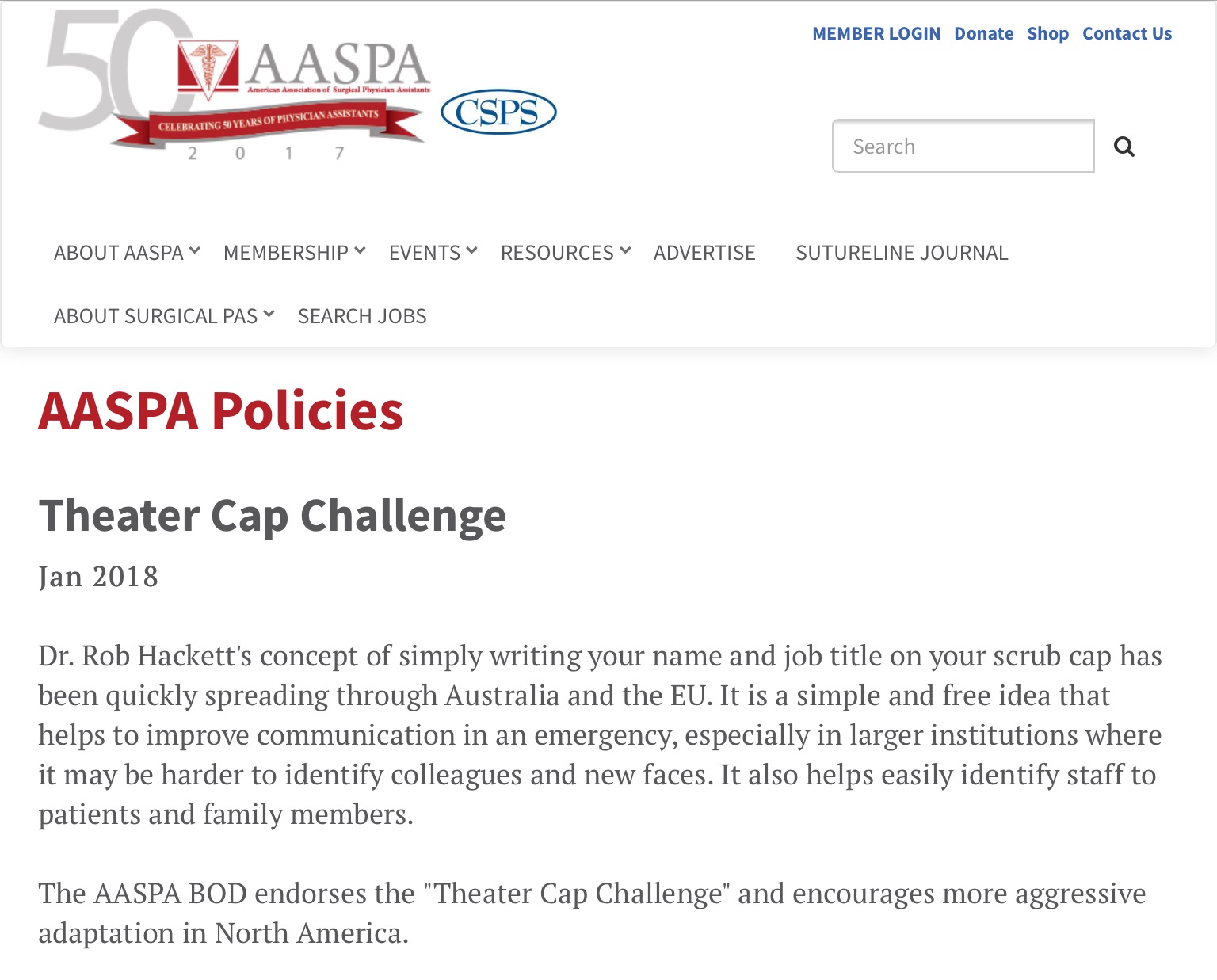
- Endorsed by American Association of Surgical Physician Assistants
- Australia and New Zealand College of Anaesthetists Bulletin
- Support from the European Society of Anaesthesiology and the American Society of Anesthetisology
- Chris Pointon #hellomynameis
Infection Control
- Haskins IN, et al. Hernia. 2017.‘There is no association between the type of surgical hat worn and the incidence of postoperative wound events.’
- Hussain S, et al. Neurosurgery, Volume 82, Issue 4, 1 April 2018, Pages 548–554.‘Mandatory Change From Surgical Skull Caps to Bouffant Caps Among Operating Room Personnel Does Not Reduce Surgical Site Infections in Class I Surgical Cases.’
- Markel T et al, Journal of the American College of Surgeons. October 2017. Volume 225, Issue 4, Supplement 2, Pages e29–e30‘When compared to cloth skull caps, disposable bouffants had greater permeability, greater particulate contamination, and greater passive microbial shed.’
- Kothari SN, et al. Journal of the American College of Surgeons. 2018.‘Attending surgeon preference for bouffant vs skull cap does not significantly impact SSI rates after accounting for surgical procedure type.’
- Elmously et al. Journal of the American College of Surgeons. 2018.Implementation of the AORN guidelines has not decreased SSIs and has increased healthcare costs.
- Journal of Hospital Infection 2002 – There is no need for non scrubbed theatre staff to wear disposable headgear
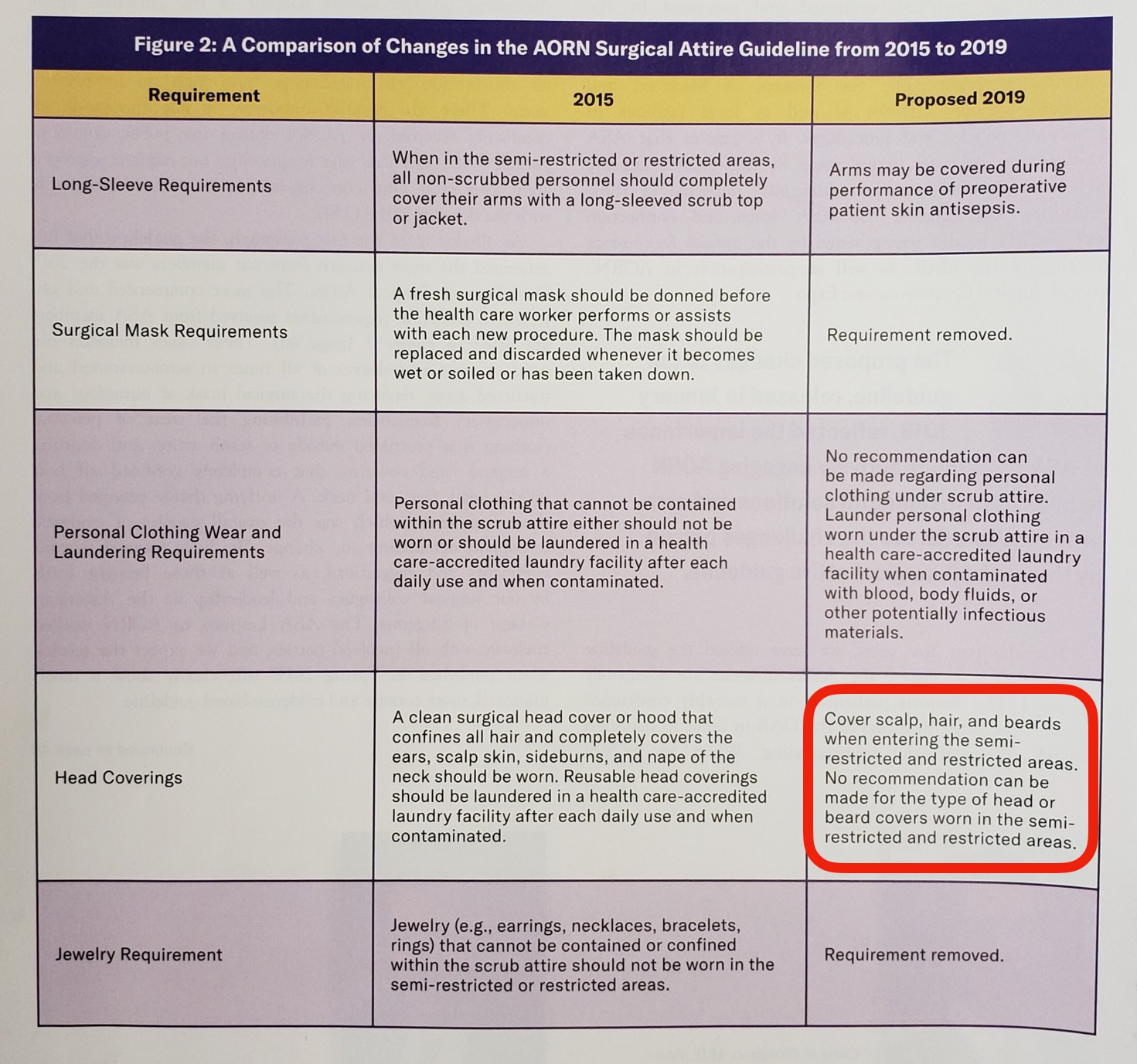
Policy review
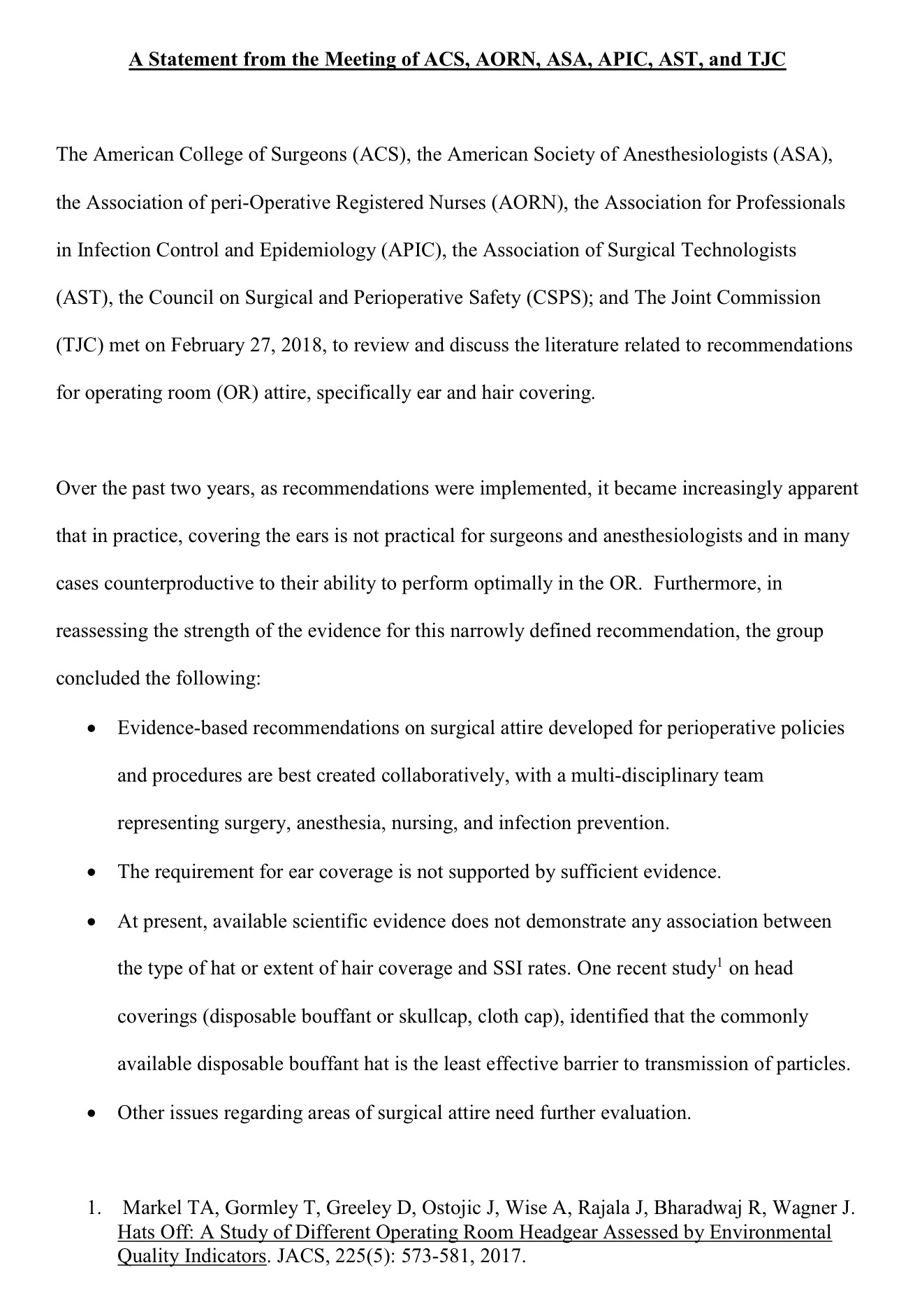
- Collaborative statement from AORN, ACS, ASA, APIC, AST and TJC – at present available scientific evidence does not demonstrate any association between the type of hat and SSI rates.
- ACORN standards reference Australian Standards which don’t actually relate to headwear.
- Excellent review of ACORN Standards as they relate to theatre caps by Dr Rhys Thomas
- Information for Trusts about TheatreCapChallenge hats – Draft policy presented to Royal College of Surgeons by Mrs Scarlett McNally
Environmental Benefit
- 20 theatre hospital discards approximately 100,000 disposable theatre hats every year. These hats are made from viscose – a substance whose production is particularly harmful to the environment:
- From ANZCA PS64 (Statement on Environmental Sustainability in Anaesthesia):Use of reusable surgical gowns, dedicated operating theatre footwear and freshly laundered lint free hats will reduce the amount of single use gowns, caps and overshoes that are discarded and add to waste.
- Results showed that that the reusable scrubs have considerably lower environmental impact within the studied categories. The main reason for this is the longer lifespan of the reusable garments, which results in substantially decreased environmental impacts per use within all phases of the lifecycle except usage.
Financial benefit
- ‘I looked at the number of hats that were purchased over a 12 month period. This came to >93,000 hats per year at a cost of NZ$14,600 (AUD 13,410). We have 15 theatres and 430 staff members (includes all surgeons / anaesthetists and surg/anaes registrars).’ – Broadbent J.
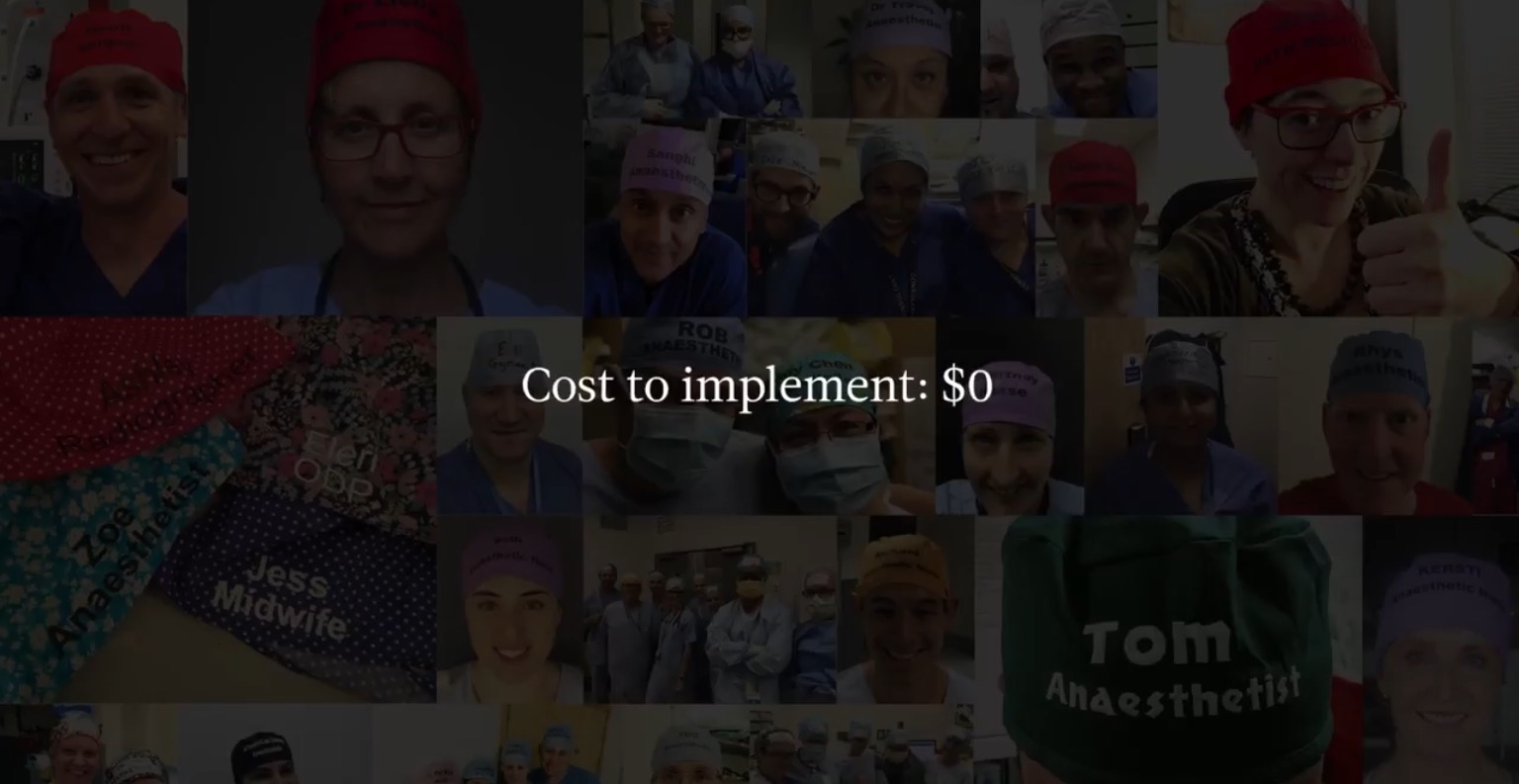
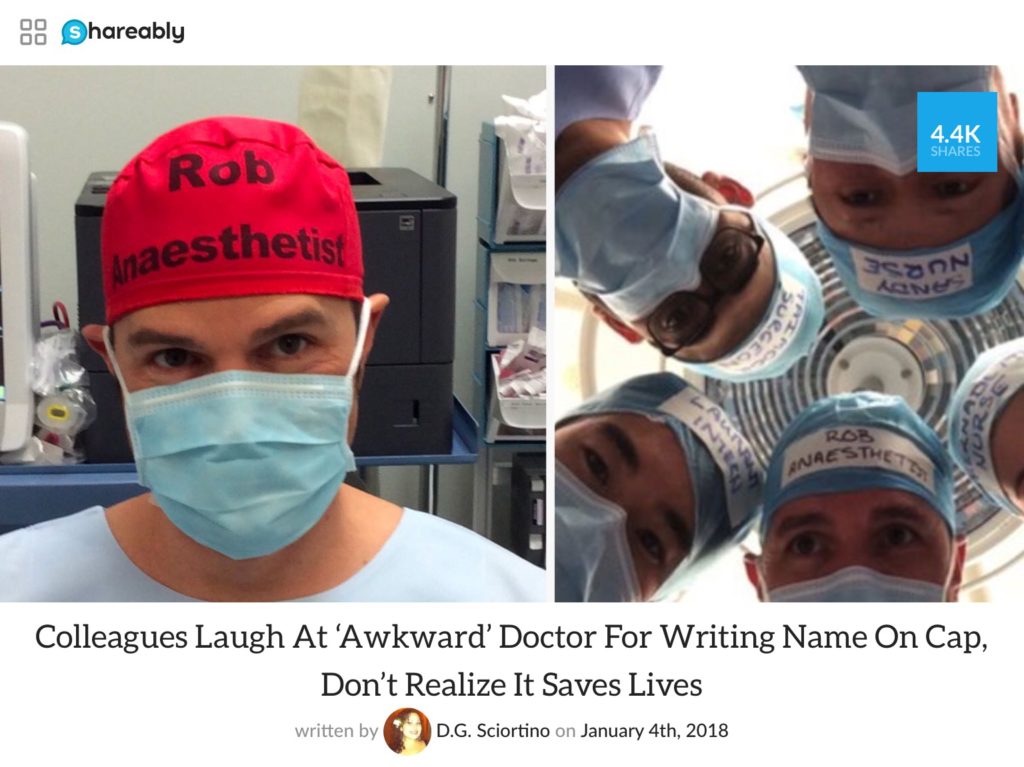
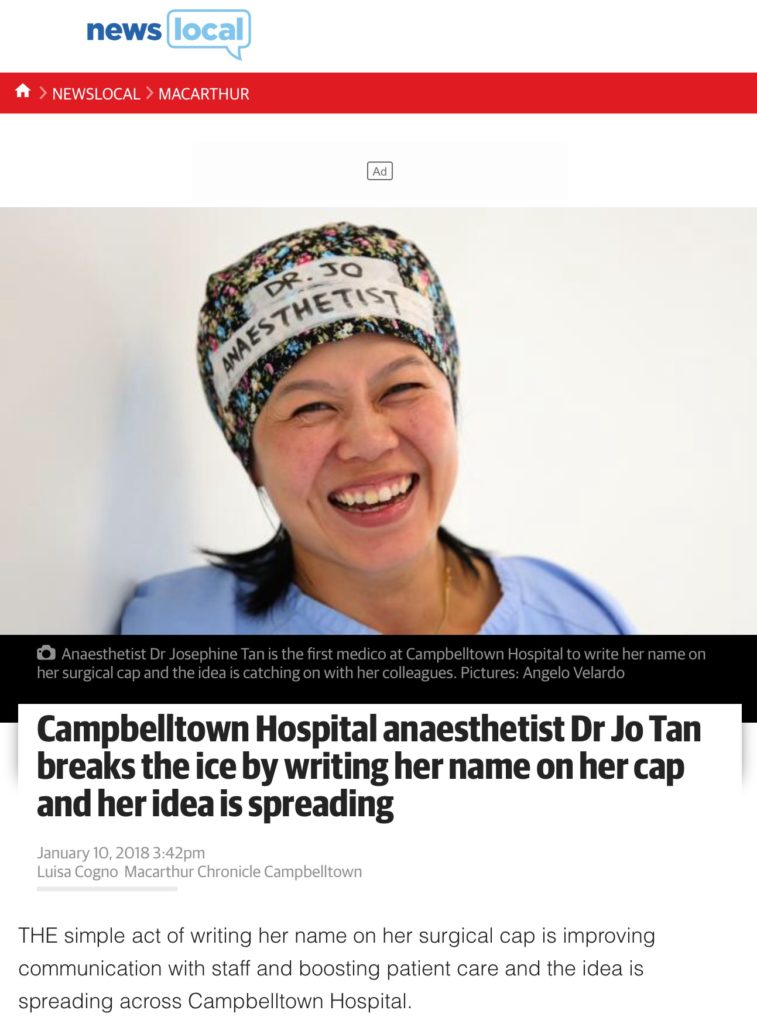
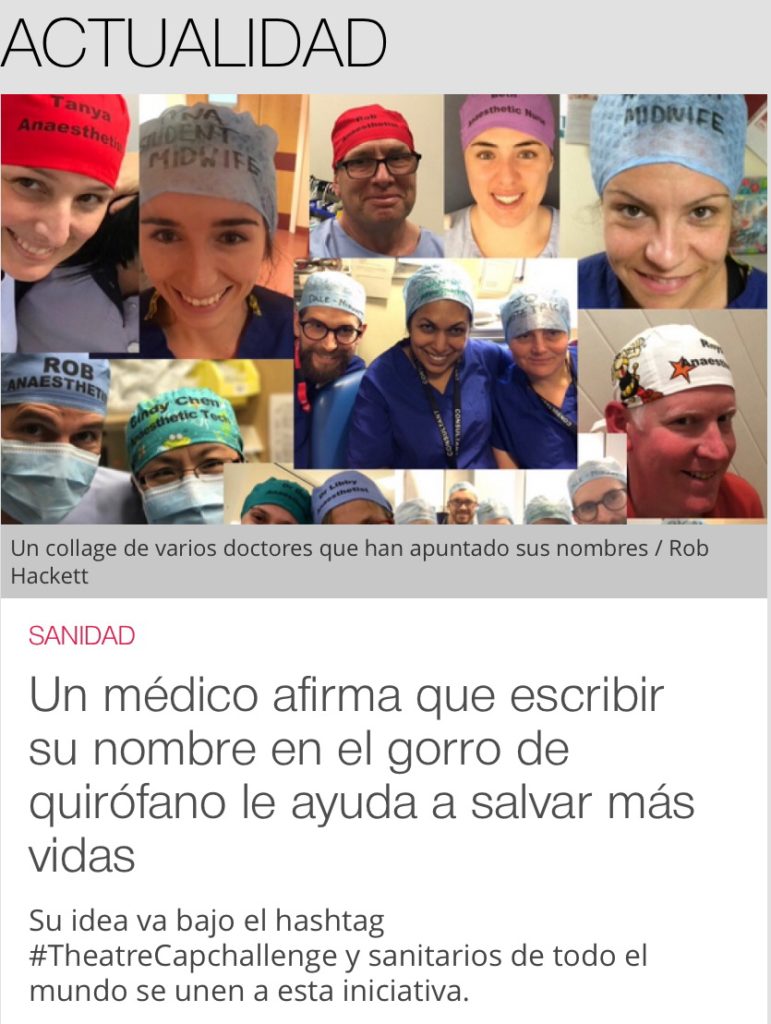
Mainstream media support
Its great to see so many hospitals across the world taking on the initiative. We continue to add to this map of hospitals where staff have shown their support (please look at the very bottom of this post for image gallery – keep sending your images through and we’ll add them and add to the map):
[huge_it_maps id=”9″]
Please watch these brief videos which provide some background & data for name & role theatre caps:
#TheatreCapChallenge – Back to Why – Part 1:
#TheatreCapChallenge – Back to Why – Part 2:
#TheatreCapChallenge – Back to Why – Part 3:
For those unsure that clearly displaying ones name and role will improve communication, teamwork and patient outcomes this information may help:
Communication errors have been implicated as the root cause of nearly 70% of adverse events (see here). Further studies have demonstrated communication failures occur in approximately 30% of theatre team exchanges and a third of these have immediate effects such as causing innefficiency and tension (see here).
Is staff misidentification an issue?
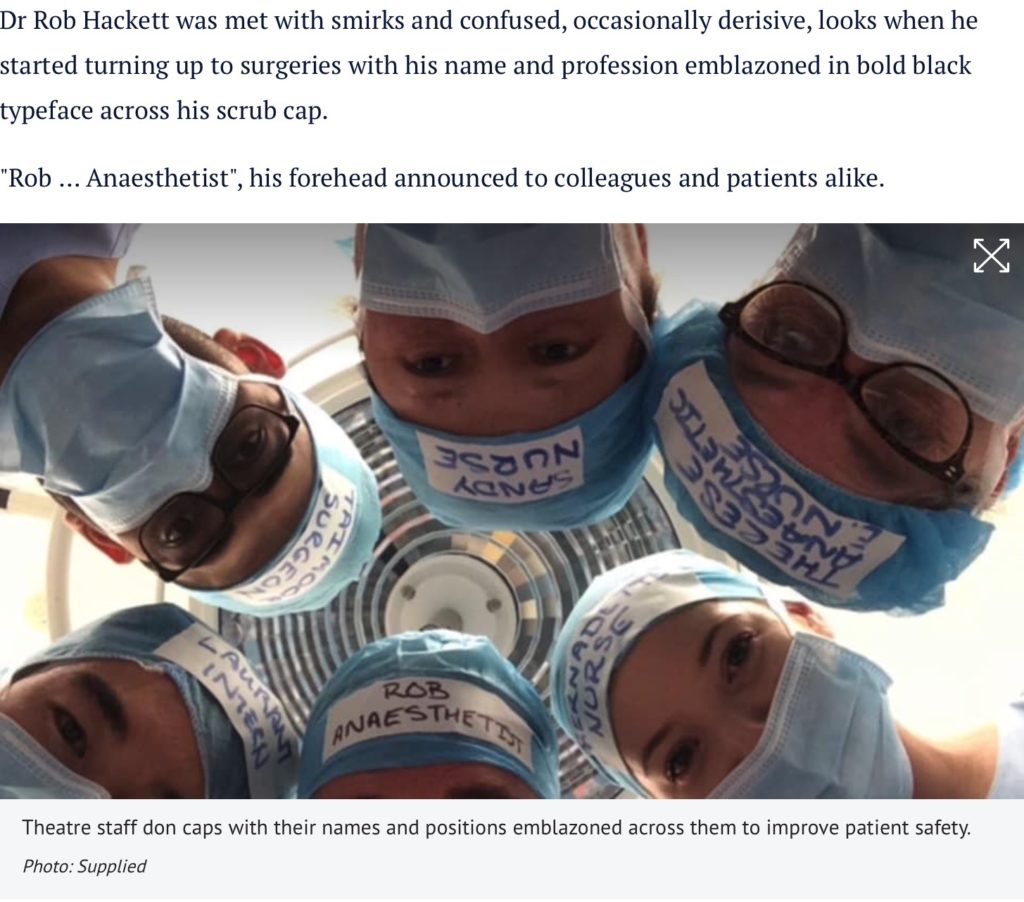
Staff misidentification can lead to significant adverse outcomes. There are numerous reports – perhaps most concerning was an anaesthetist believing a staff member to be a nurse qualified in checking blood allowing blood to be given. Unfortunately the staff member was a theatre porter, the wrong blood was given and the patient died. Staff misidentification was felt to be a major contributory factor (see here).
Cocktail Party Effect
Through the use of a persons name we are able to focus them and then their attention towards a specific task (see here).
How good are doctors at introducing themselves? (see here)
Theatre staff are notoriously poor at completing the name & role part of the Team Time Out (see here)
How good are humans at remembering names?
Humans only recall 30% of names after first introduction. After introduction we are much more likely to remember someone’s profession eg baker than their name Mr Baker (see here).
We are also very poor at remembering names after we have learnt them, being much more likely to remember faces (see here).
How well do theatre staff recall names after the team brief?
25% of surgeons did not know the scrub nurses name and 30% of surgeons did not know the anaesthetists name (see here).
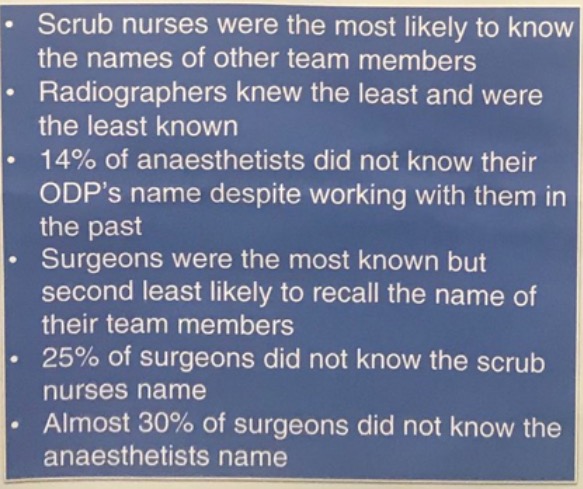
The surgeon only knew 44% of staff names in theatre (see here).
we are awaiting the publication of data from Professor Marlies Schivjen and the Black Box Europe team. Marlies is a professor of communication based in Amsterdam:

The number of different combinations of staff constituting the team attending a critical patient event (eg an obstetric emergency) in a single hospital can be in the 100s of millions (see here).
Knowing and recognising team members by name has been quantitatively and qualitatively associated with increased trust, work engagement and clinical improvement (see here).
An RCT which demonstrates that wearing hats would lead to prevention of patient deaths require over a million patients in either limb. This is because because of the frequency of the event rate eg death from anaesthesia is so low, not because of lack of effectiveness from the intervention (see here). We need to look at other end points.
In 2008 the Garling Enquiry stated all healthcare staff should wear badges or similar bearing in large print the person’s name and title or role.
A brochure produced by NSW Health in response to the Garling Enquiry (click on image, page 7):
How else might we Trial the impact of name & role theatre hats on patient safety?
Perhaps through using surrogate markers such as time to defibrillate a patient in a simulated scenario comparing staff with and without obvious identification (see here).
Qualitative blinded review assessment of simulated theatre teams comparing those displaying their name and role against those who don’t (see here).
‘The response during this simulation was the most efficient and effective of any simulation we had ever run. In particular, we found communicating directly by first names enhanced the participant’s ability to have closed-loop communication.’ (see here)
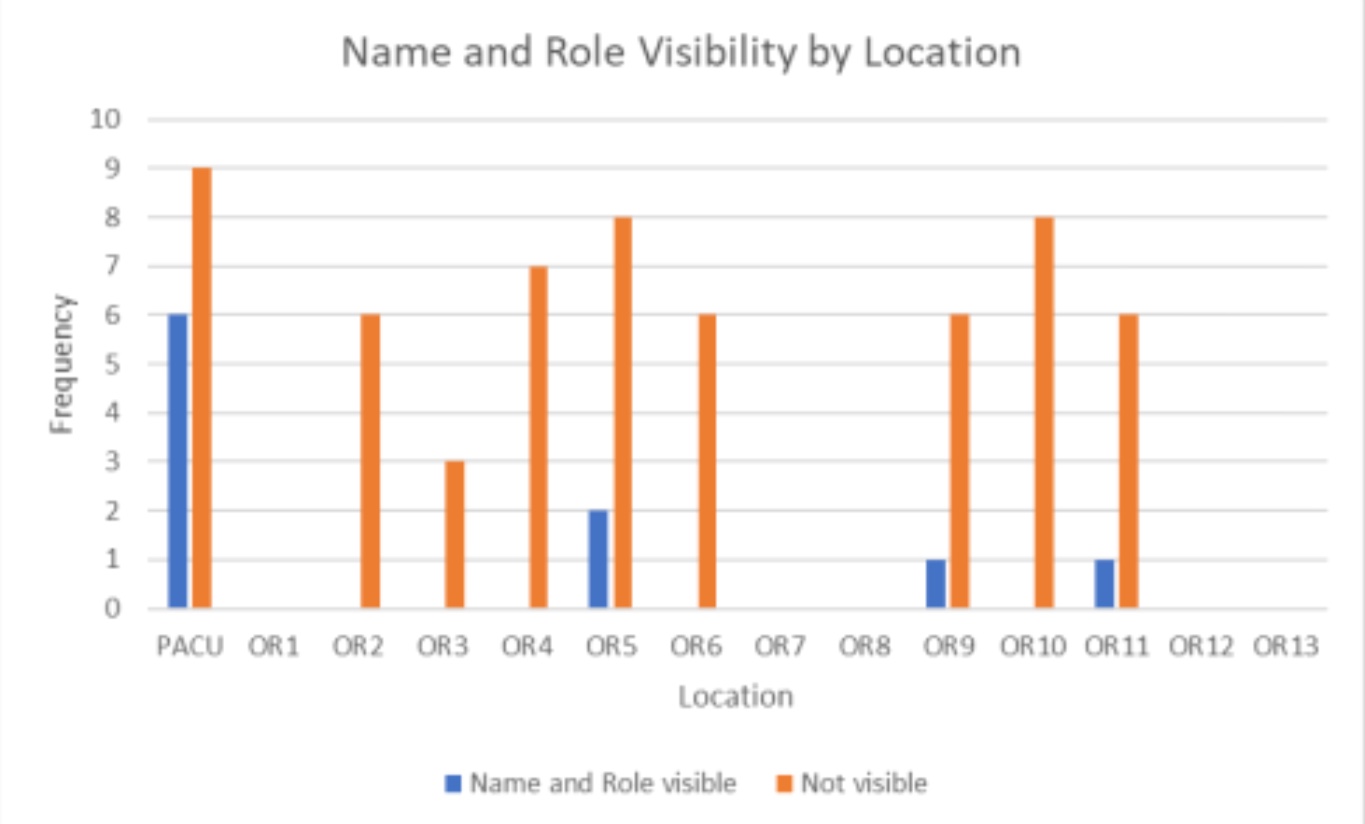
Survey data from pre and post implementation of name and role theatre hats with many thanks to David Kinnersley (see here) – slides below demonstrating data obtained pre and post name and role hat implementation:
What’s in a name
Fantastic presentation by Dr Rhys Thomas – Quality & Safety Fellow John Hunter Hospital. He discusses how name badges on tops in theatre are often covered up by sterile, lead or warming gowns, how writing names on a whiteboard is often ineffectual and much more (see here).
#TheatreCapChallenge in the BJA – click on image for link:
Improved patient outcomes & recovery when their own name is used during emergence from anaesthesia (see here).
If ACORN Standards (or similar) are being innapropriately used at your institution to prohibit the use of reusable theatre hats please read and share this post: see here – if we want better patient care we may need to break the rules.
Re-usable hats may be superior to disposable bouffant hats for infection control
Evidence indicates there is no difference in infection rates between cloth reusable and disposable hats (see here, see here). Further evidence indicates no difference in infection rates when strict hat policies introduced which required covering of ears (see here). Further based on dynamic operating room and fabric assessment cloth hats appear to be superior to disposable bouffant hats (see here).
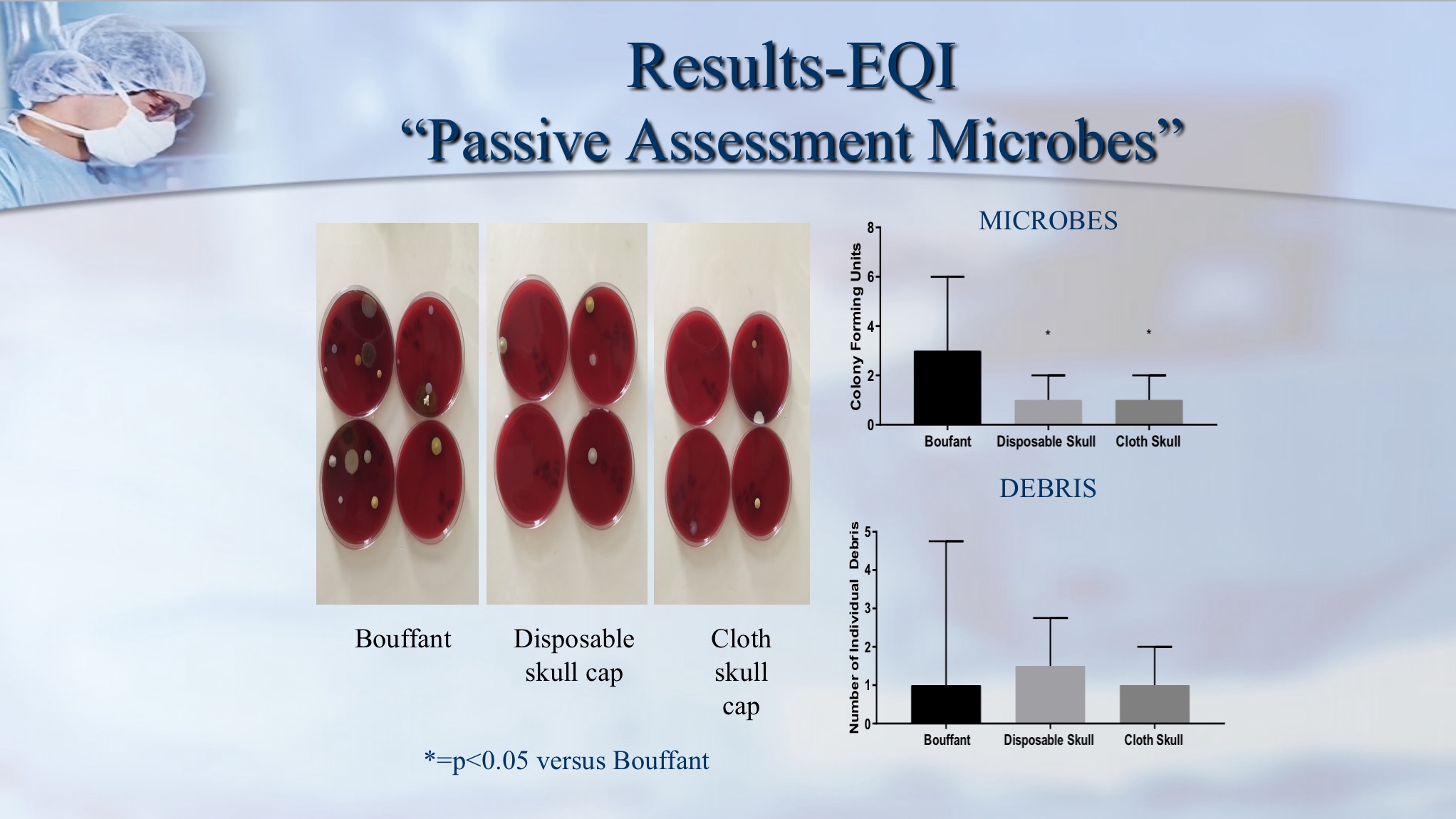
In America a collaborative meeting amongst the main governing bodies in February 2018 concluded that ‘At present, available scientific evidence does not demonstrate any association between the type of hat or extent of hair coverage and SSI rates’
The wearing of disposable theatre caps appears over time to be an ingrained ritual with no evidence supporting this practice from an infection control perspective. Click on image to read more:
Re-usable hats are also better for the environment:
From ANZCA PS64 (Statement on Environmental Sustainability in Anaesthesia): Use of reusable surgical gowns, dedicated operating theatre footwear and freshly laundered lint free hats will reduce the amount of single use gowns, caps and overshoes that are discarded and add to waste.
Disposable hats are manufactured from ‘viscose’ – a substance whose production is of significant detriment to the environment (click on image below to read more):
Reusable hats may also represent a significant cost saving:
‘I looked at the number of hats that were purchased over a 12 month period. This came to >93,000 hats per year at a cost of NZ$14,600 (AUD 13,410). We have 15 theatres and 430 staff members (includes all surgeons / anaesthetists and surg/anaes registrars).’ – Broadbent J.
Where staff cover own costs/hats bought for them eg through sponsorship then this could represent a significant front end cost saving each year for that hospital. There will also be major environmental benefits.
It would be difficult to workout further cost savings from increasing theatre efficiency and patient outcomes.
Given re-usable hats have many advantages over disposable ones why does my hospital not allow them?
Practices maintained through a command structure often go unchallenged through fear. They can be perpetuated and reinforced for years – read a very amusing example here – signing a bicycle register at one hospital for those who rode their bikes to work. The register originated in the days of rationing and was of no relevance for the next 60 years – however it persisted because of the command structure (see here).
Within Australia the ACORN standards and hat washing requirements are often inappropriately used as a barrier to name & role theatre hats. Please read this excellent review of the ACORN standards by Dr Rhys Thomas (click on image):
For those facing resistance to the #TheatreCapChallenge in their own hospitals we’ve put together a word document you may wish to amend and provide as a letter to those resisting within your own institution: (click here)
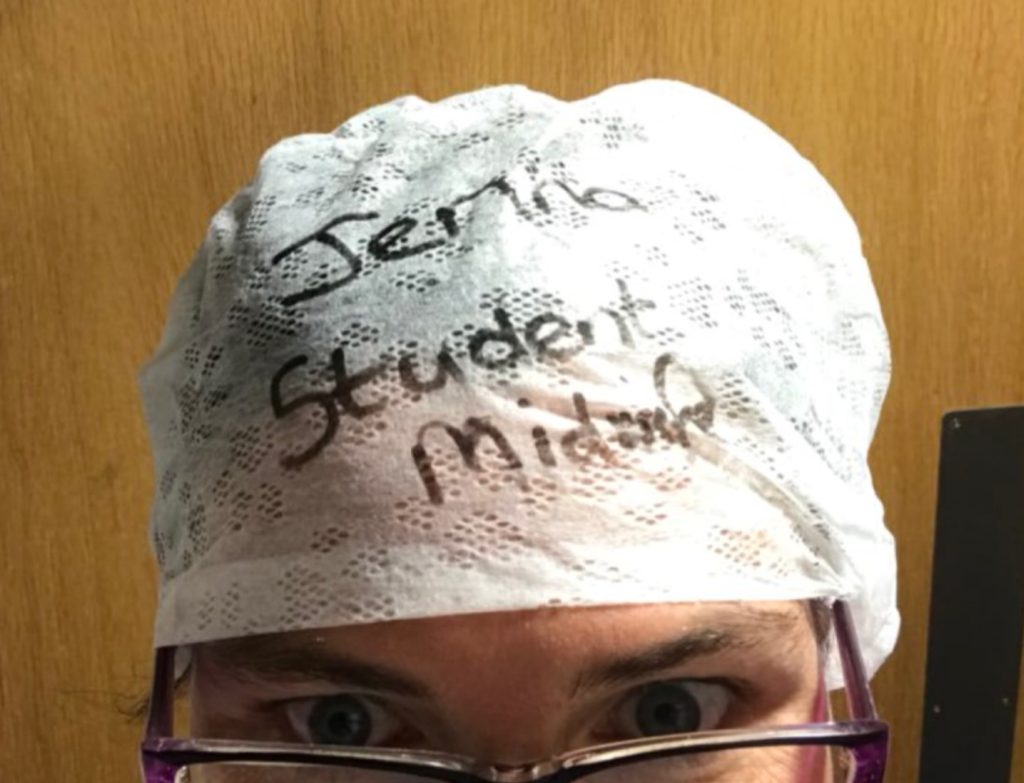
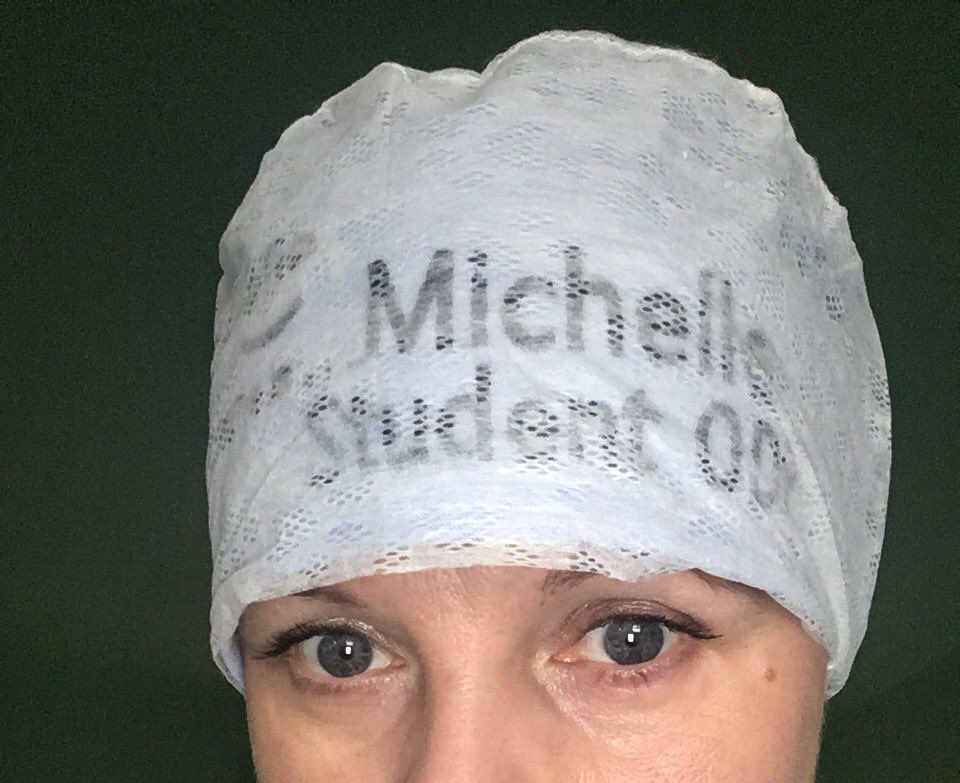
For those still facing resistance Michelle provides another option here – a disposable hat over a light coloured reusable hat which allows the dark font to show through:
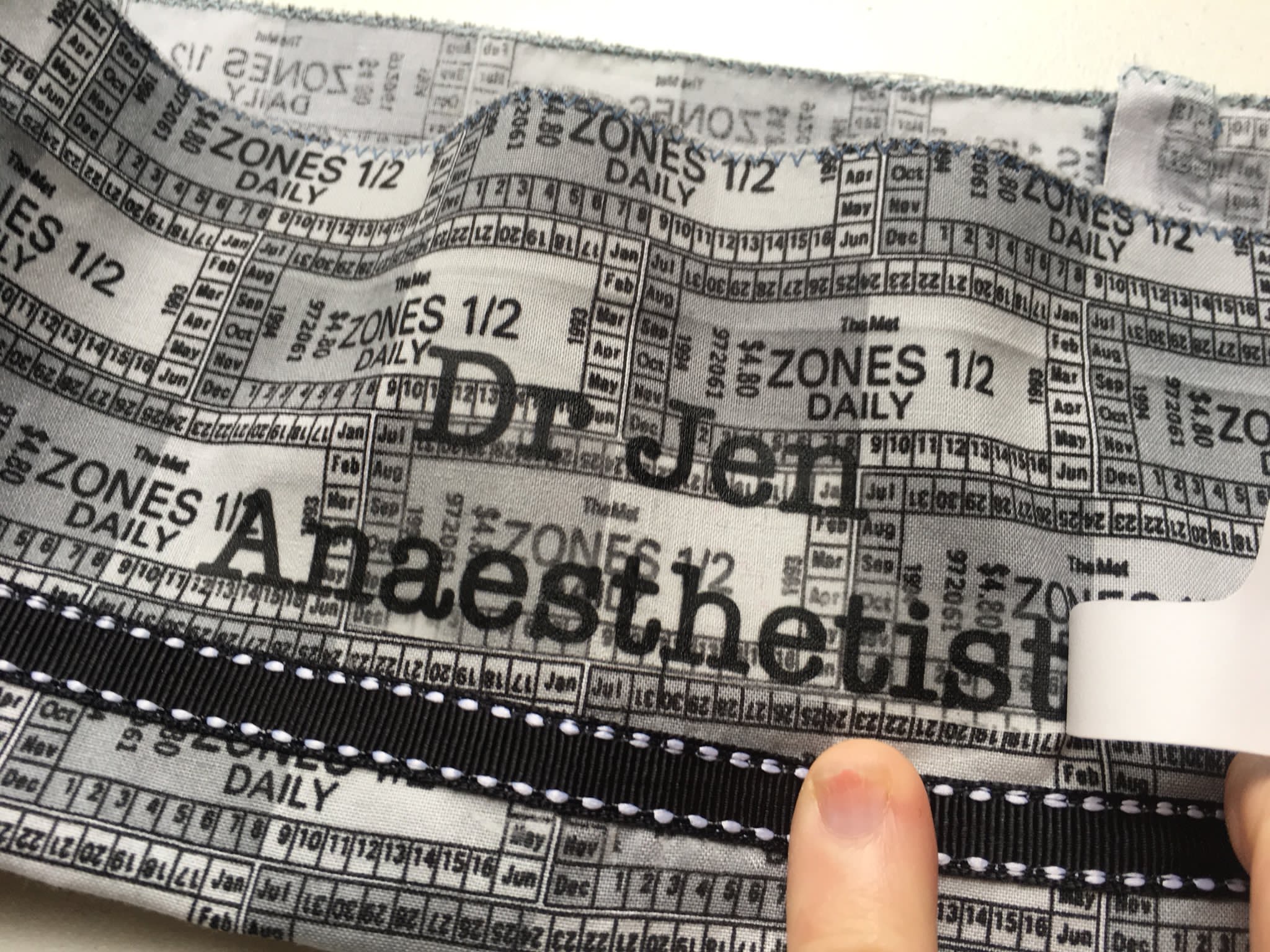
For those who already own their own hats and would like great step by step instructions on putting on iron on transfers check out this from Dr Jennifer Dixon (click on image)
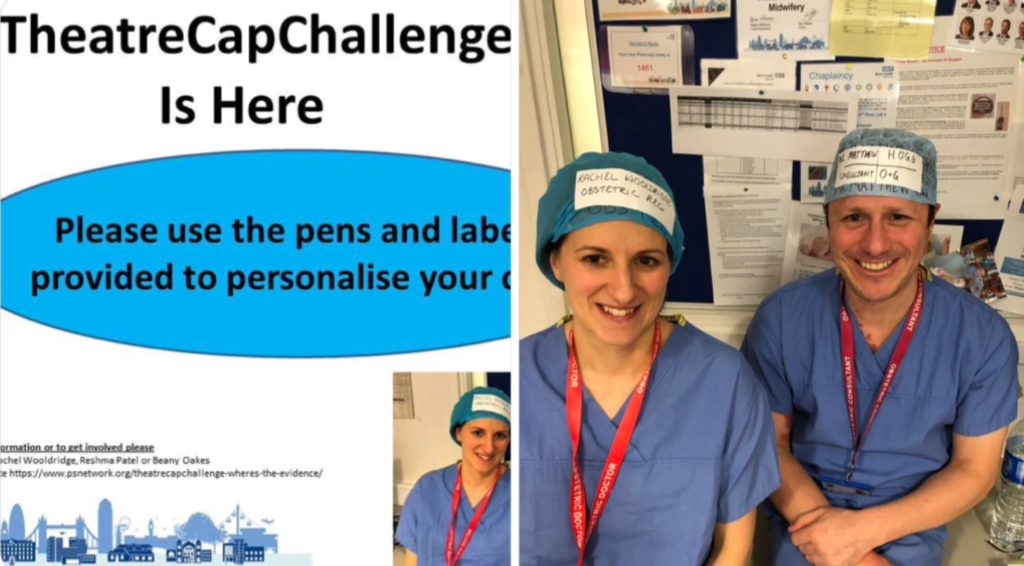
For those who would still prefer to use disposable hats there are several options:
The appearance of marker pen on hat unless well written may not be aesthetic enough for the tastes of some. Perhaps consider using sticky adhesive labels with pre-printed names and roles – we have found Avery 99.1×38.1mm 14 per sheet addressing labels (reorder no. 936044) or general use labels (reorder no. 938209) extremely suitable. One might also consider downloading the Avery Design & Print App for free – makes it extremely easy to generate label designs.
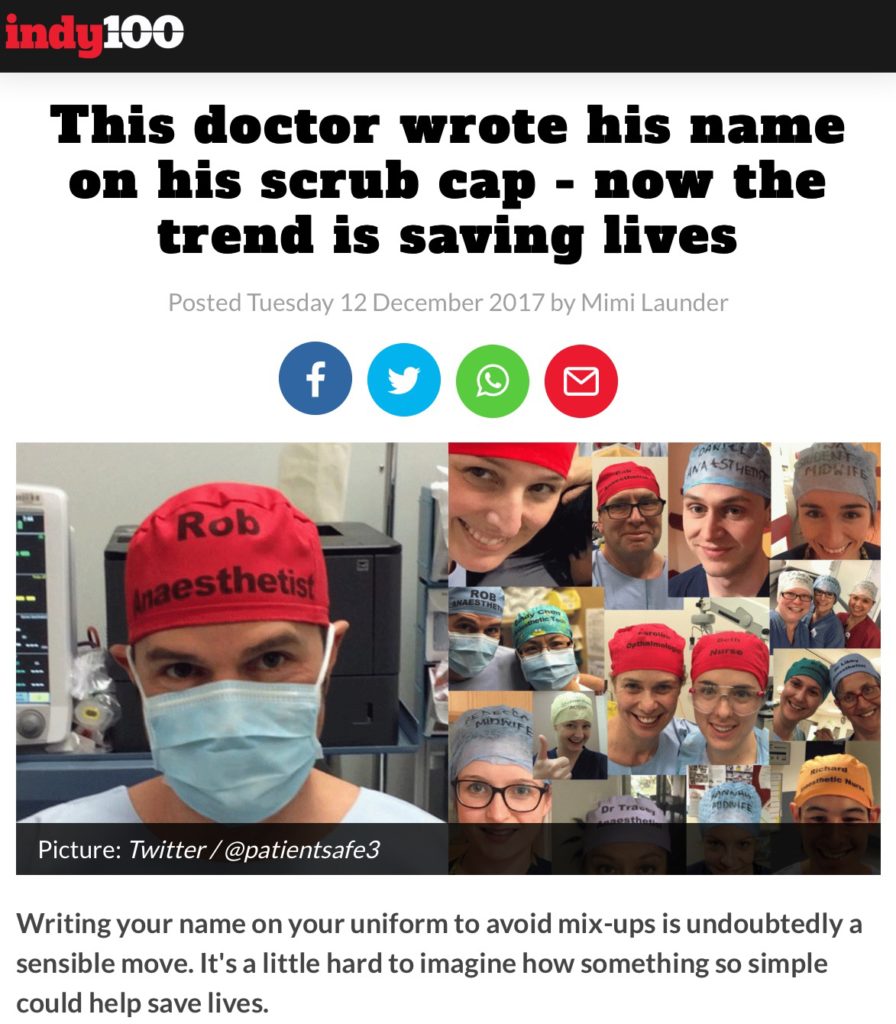
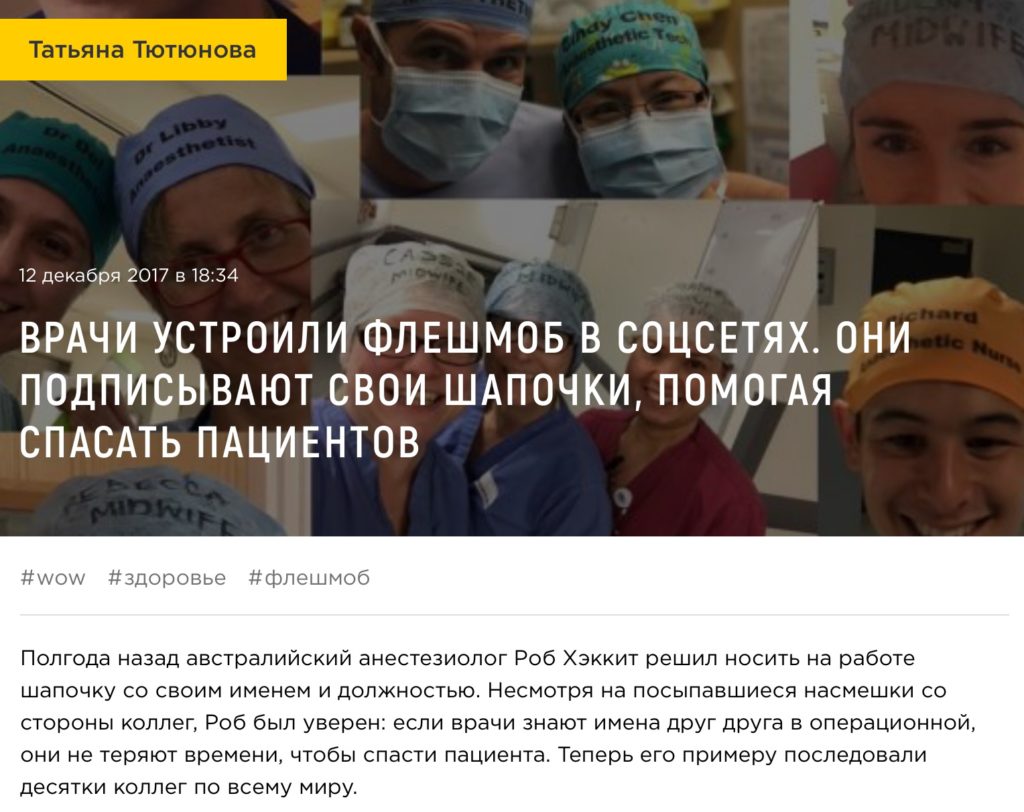
#TheatreCapChallenge in mainstream media
The #TheatreCapChallenge has been discussed in mainstream media internationally with write ups in Chinese, American, Russian, Japanese, Korean, Spanish and Indonesian newspapers. Over 2 days it was the most read article in the Sydney Morning Herald with over 1 million reads on one day, over 300,000 likes and 30,000 comments which were strongly supportive (see here).
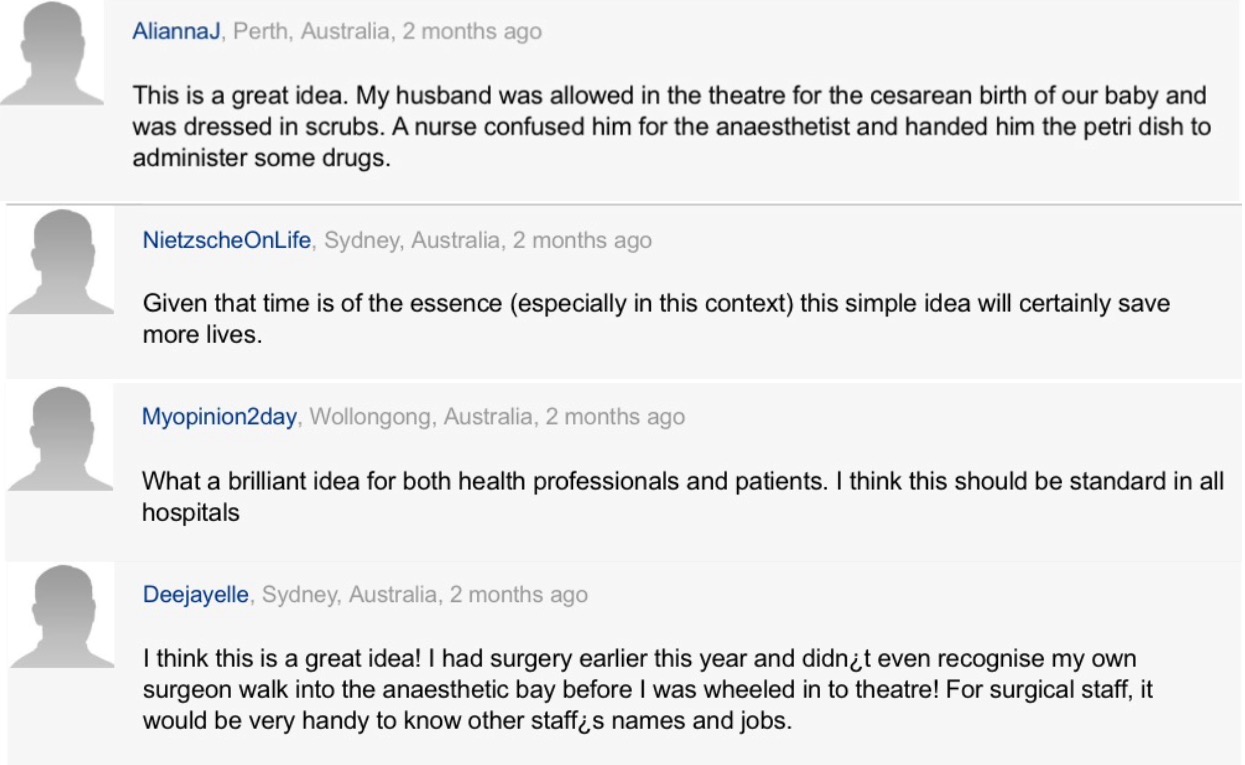
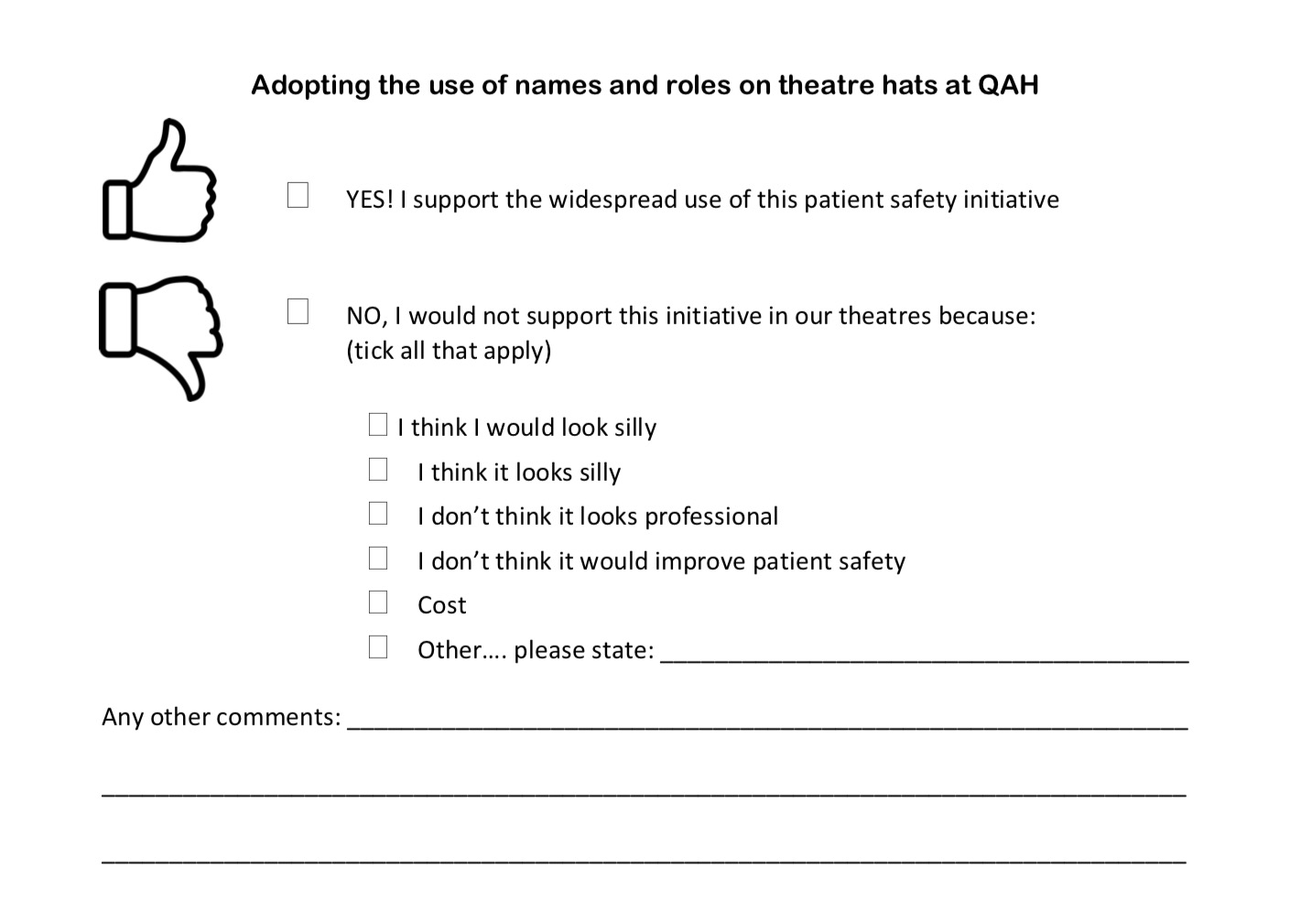
What do our front line staff think about adopting name and role theatre hats?
After a presentation explaining the implications (see here) front staff appear extremely willing to support the initiative. After handing out this questionnaire in one anaesthetic department the support was overwhelmingly supportive.
A twitter poll performed by anaesthetist Sethina during her week in charge of the @NHS :
Patient satisfaction survey from University Hospital Birmingham (click on image):
If it’s the right thing to do why haven’t name & role theatre hats been readily adopted?
Cognitive dissonance (see here) Semmelweis effect (see here). Healthcare is governed by a command structure. If endeavours aren’t fully supported by those in positions of authority the front line are extremely hesitant to adopt them (see here). Those in senior positions perhaps need to make the greatest change from being authority figures to facilitators of ideas for improvement coined on the front line.
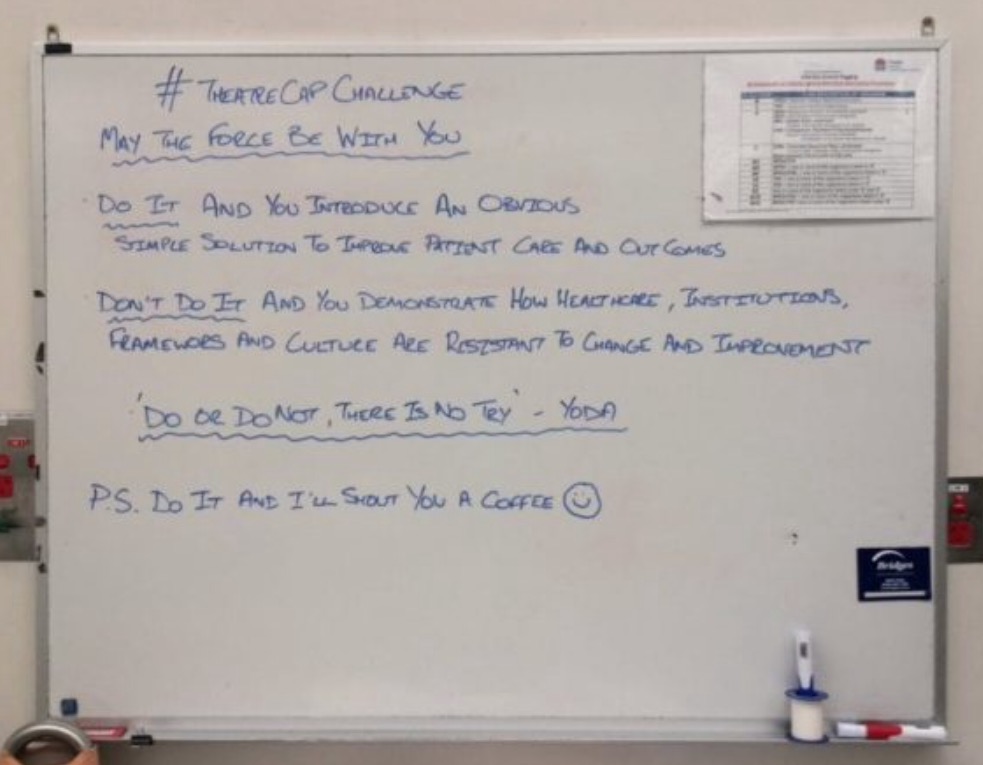
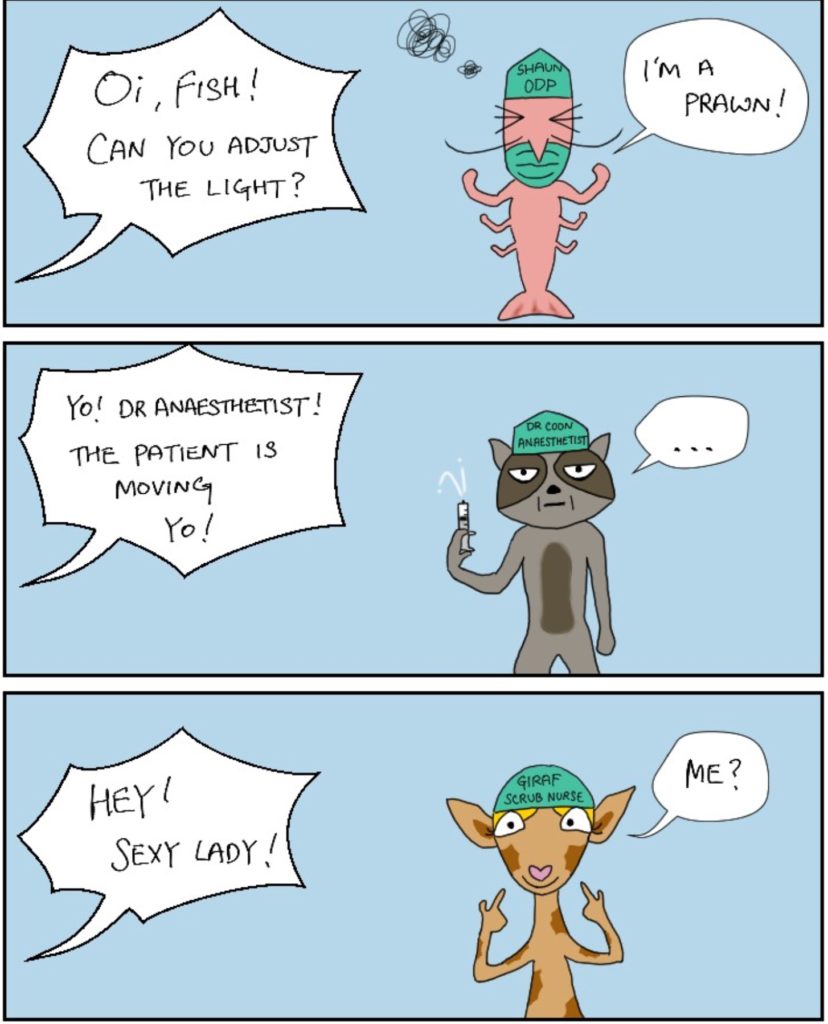
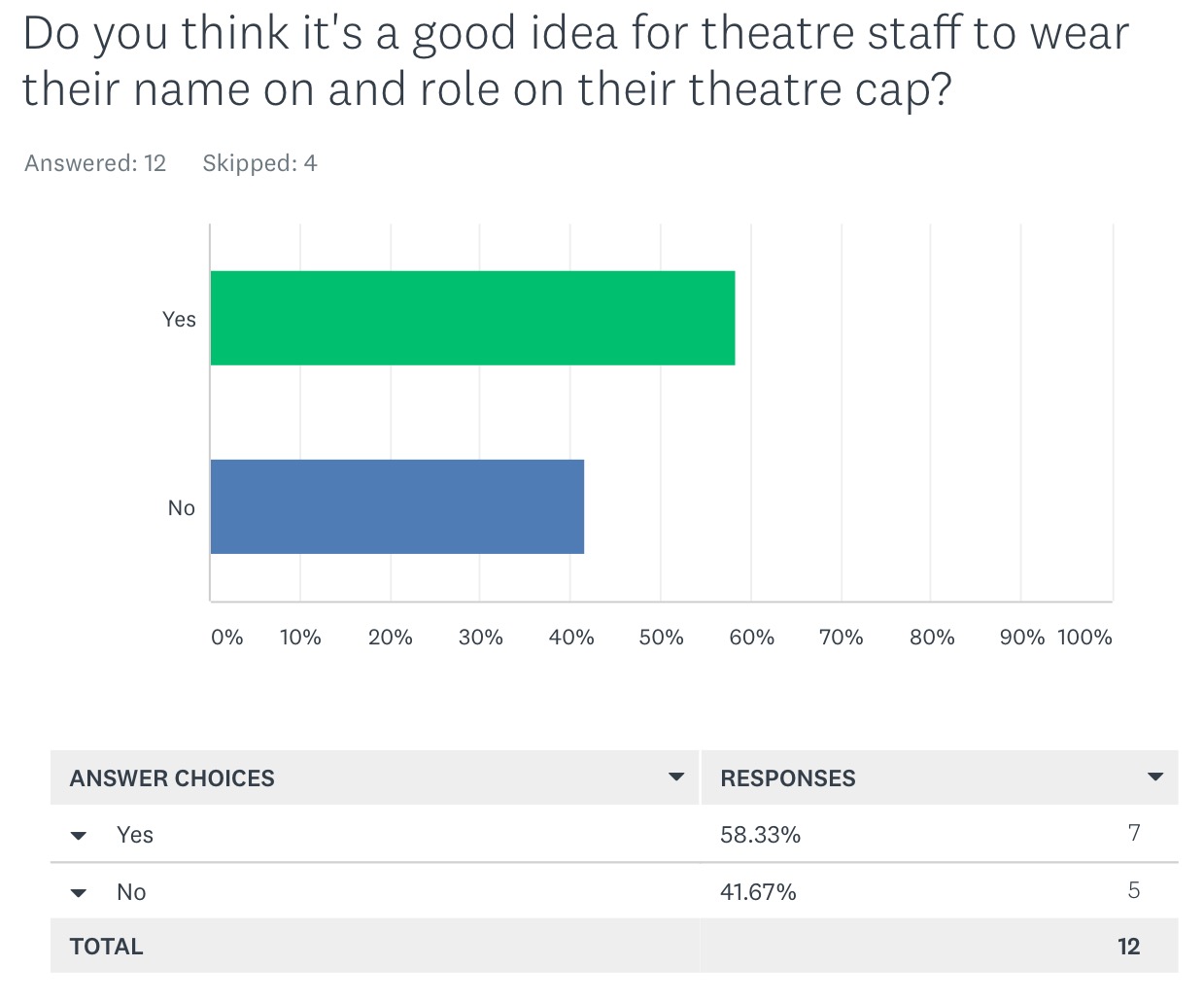
While the #TheatreCapChallenge creates a positive friendly work environment it can expose how bad current healthcare culture can be:
#TheatreCapChallenge – What’s all the fuss about?
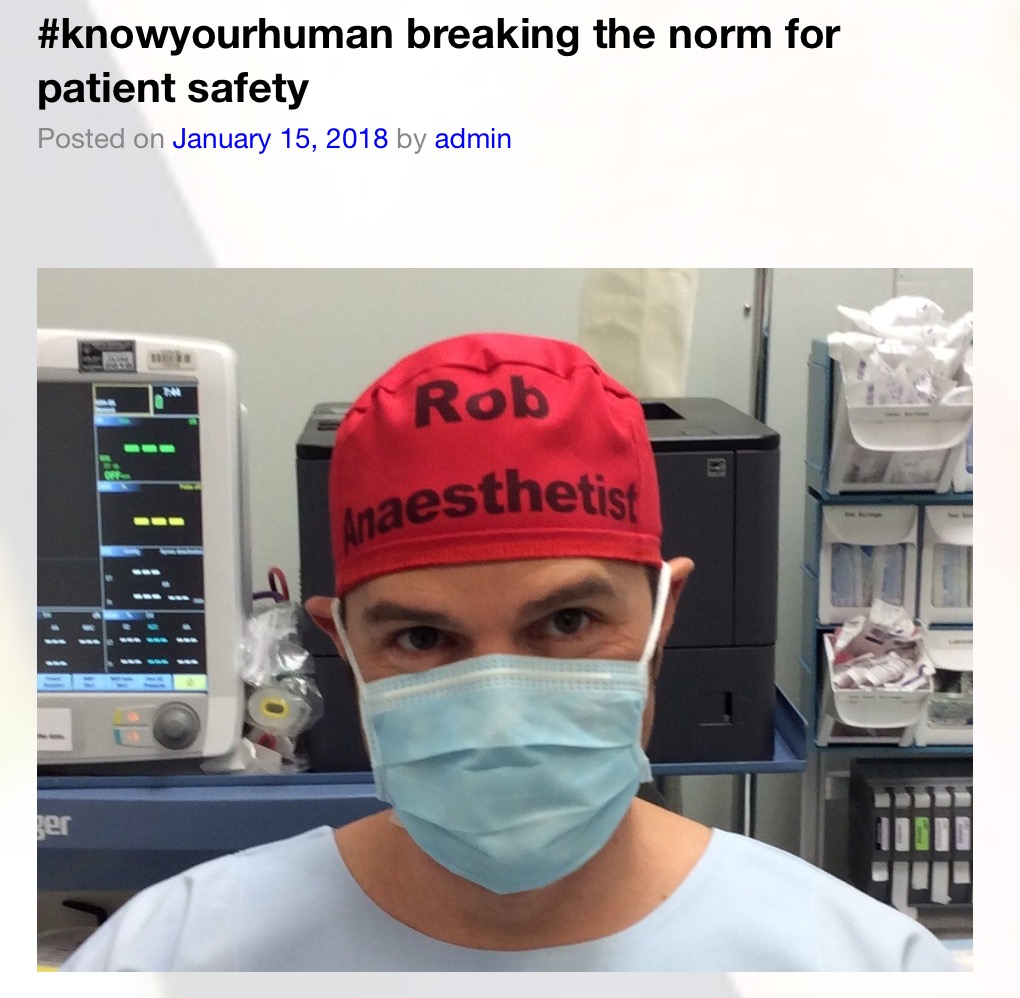
#KnowYourHuman – when we accept that we’re all human and that we all mistakes we can design our work environments to cater for this (see here)
As mad as hatter? – system safety solutions have the potential to save hundreds of thousands of lives in healthcare however trying to implement them in healthcare frameworks resistant to change can send one mad. Something has to give (see here)
Human in the Team – choose to be human and part of a team and imagine the lives you’ll save (see here)
Fixing Healthcare Safety – if safety is to improve we’ll need to understand human limitation and work together to deliver effective safety interventions (see here)
Thank You Alison Brindle – when we have a culture which truly listens to and works with front line staff to deliver their brilliant ideas then patient safety will improve. Student Midwife Alison Brindle may have found a way to deliver this culture. (see here)
Given displaying ones name and role on your person is obviously better for communication, teamwork and patient outcomes, it costs nothing to implement yet some staff still resist doing it, what is it that gets in the way? (see here)
New Kurt, New Power – Old Kurt was understandably offended when someone told him he should clearly display his name and role in theatre. It was as if someone was telling him he’d never done his job optimally. Change takes the courage to assess ones cognitive biases. In accepting it New Kurt is able to create an environment supportive of change and improvement. (see here)
Social Conformity & Groupthink – Those at the top of command structures are often the most resistant to change. Given their positions and the power of groupthink and social conformity they are able to continuously stifle initiatives even when there is overwhelming support for them to be adopted. (see here)
Great article (see here) from Alison Brindle about creating change in theatre environments through the use of social media – the power of the hashtag #TheatreCapChallenge.
From a survey of over 1000 people (the majority front line staff) there was overwhelming support for name & role theatre hats:
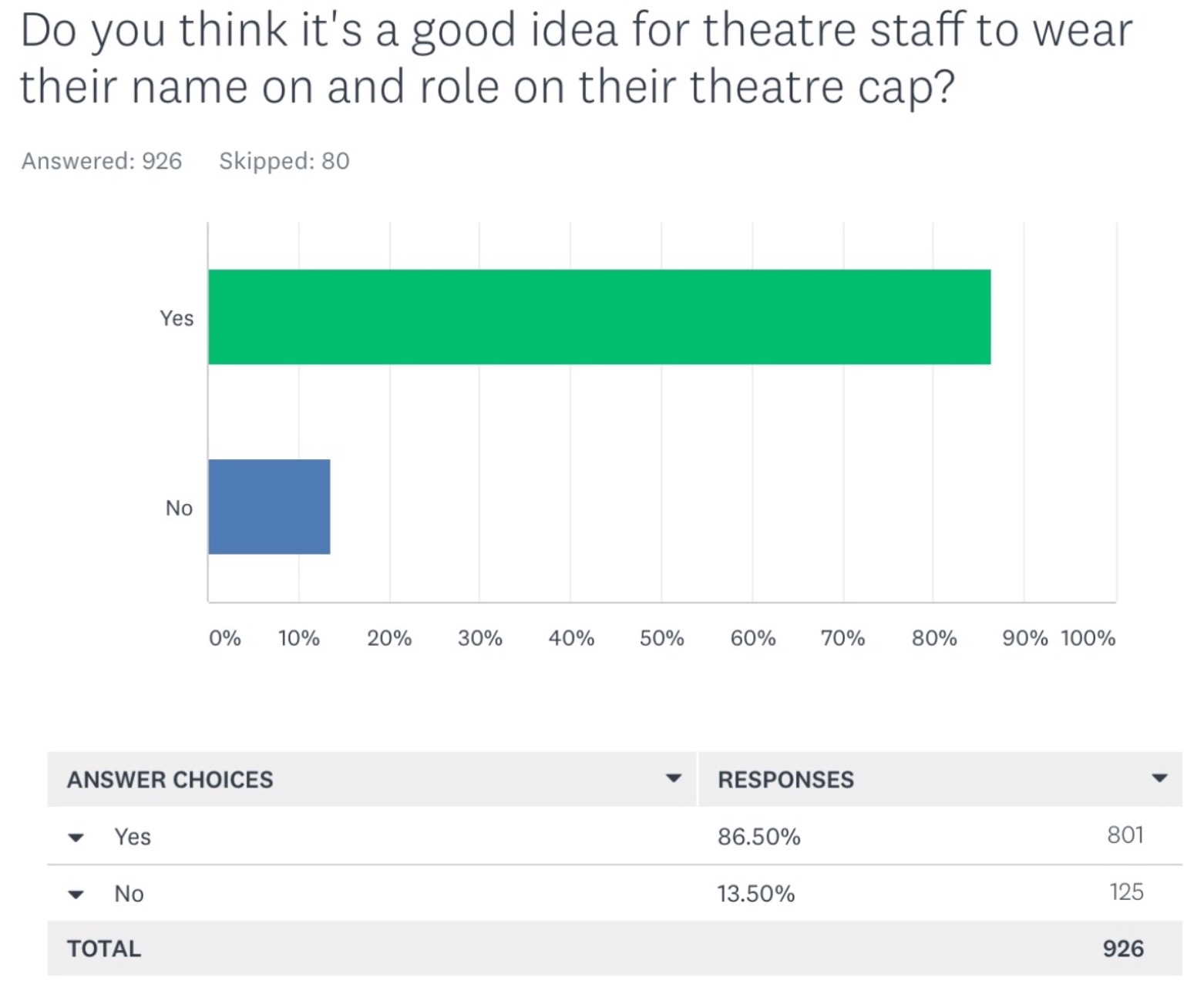
Interestingly when one looks at subgroups there is unanimous support for the initiative amongst those new to healthcare:
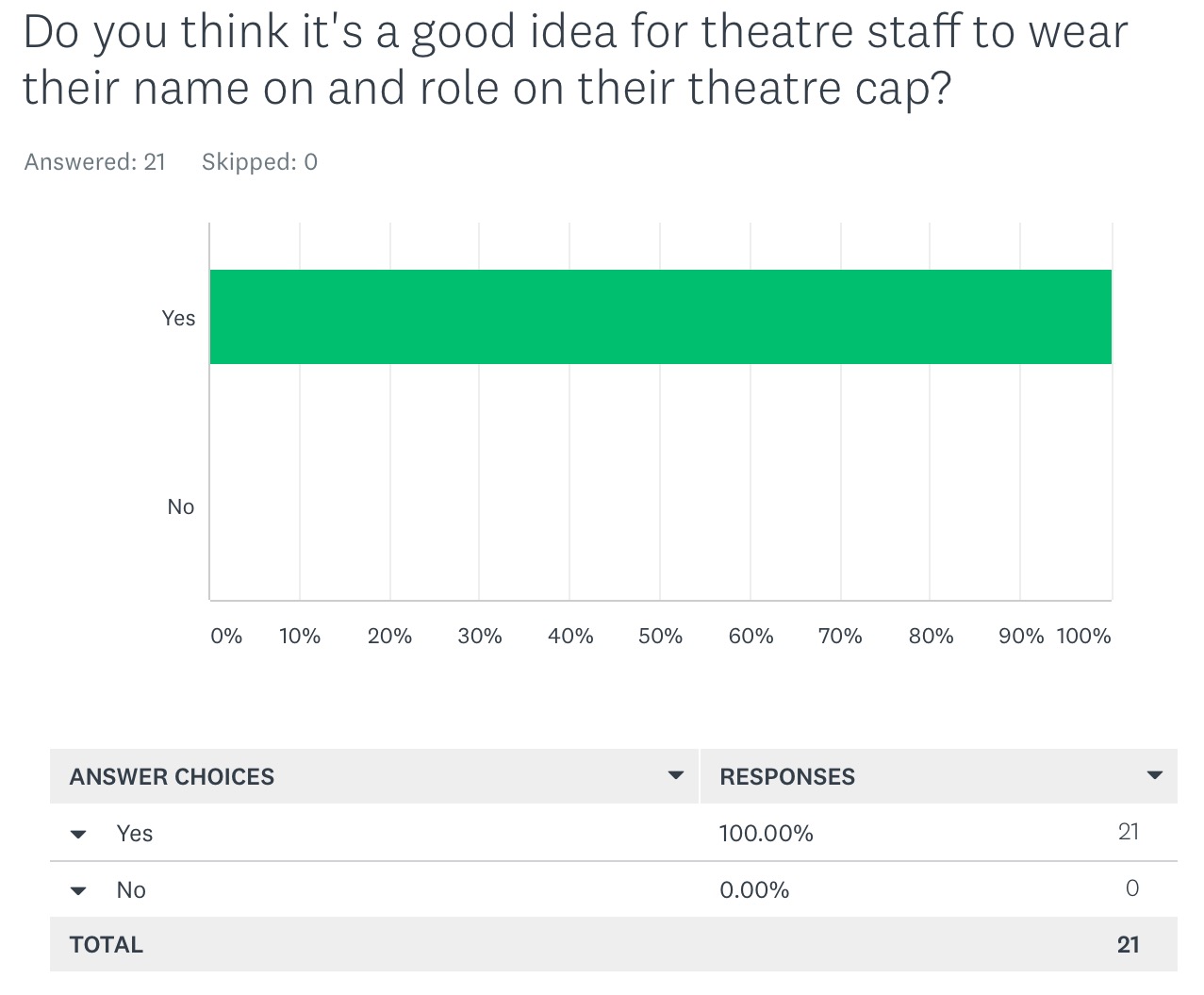
However when one looks at the data for those with the greatest influence (in this chart surgeons with more than 20 years in healthcare the data looks quite different):
Junior staff in turn are often fearful of adopting the initiative perhaps concerned about appearing disrespectful to their superiors o rather negatively impacting their own future career aspirations. In this way an obvious patient safety intervention is stifled.
This phenomenon plays out again and again in healthcare with many other suggested interventions and resultantly healthcare struggles to change and improve.
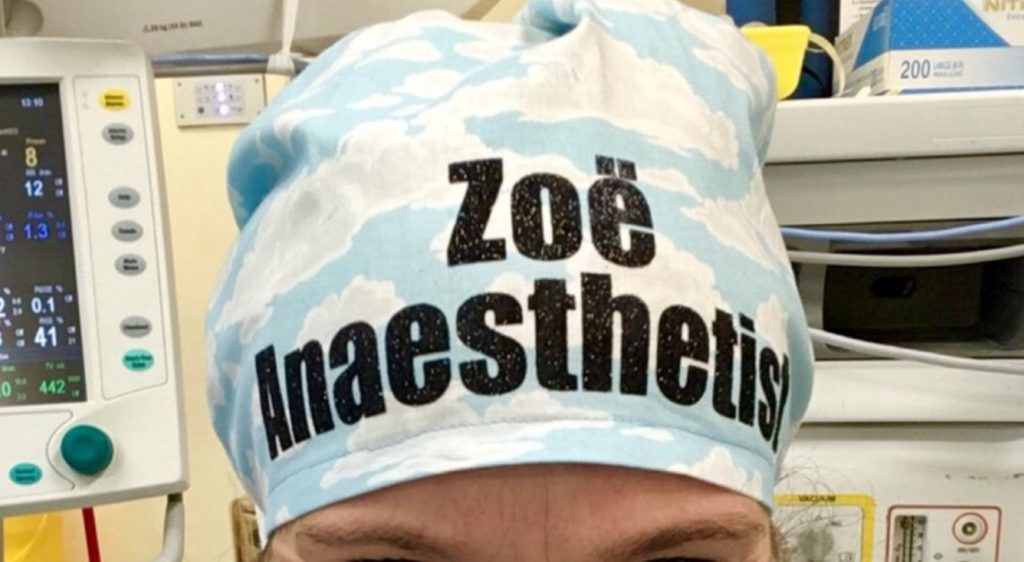
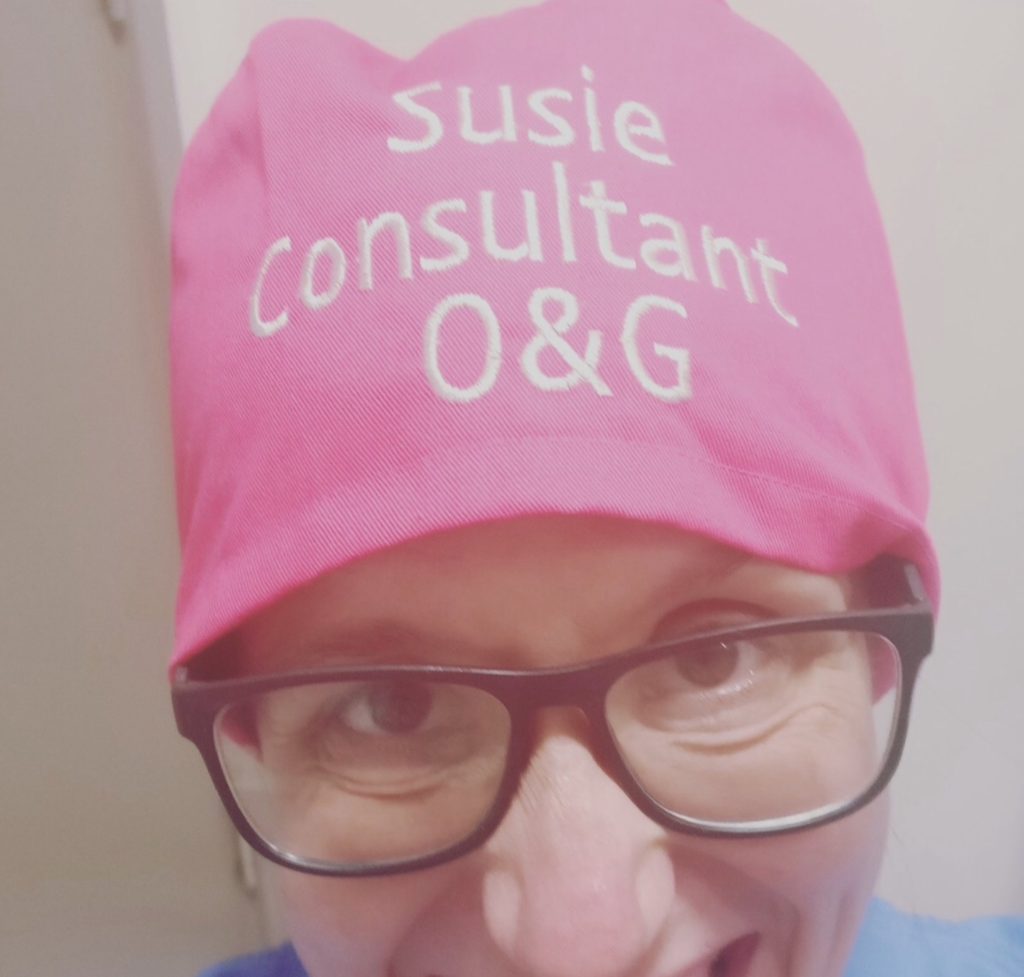
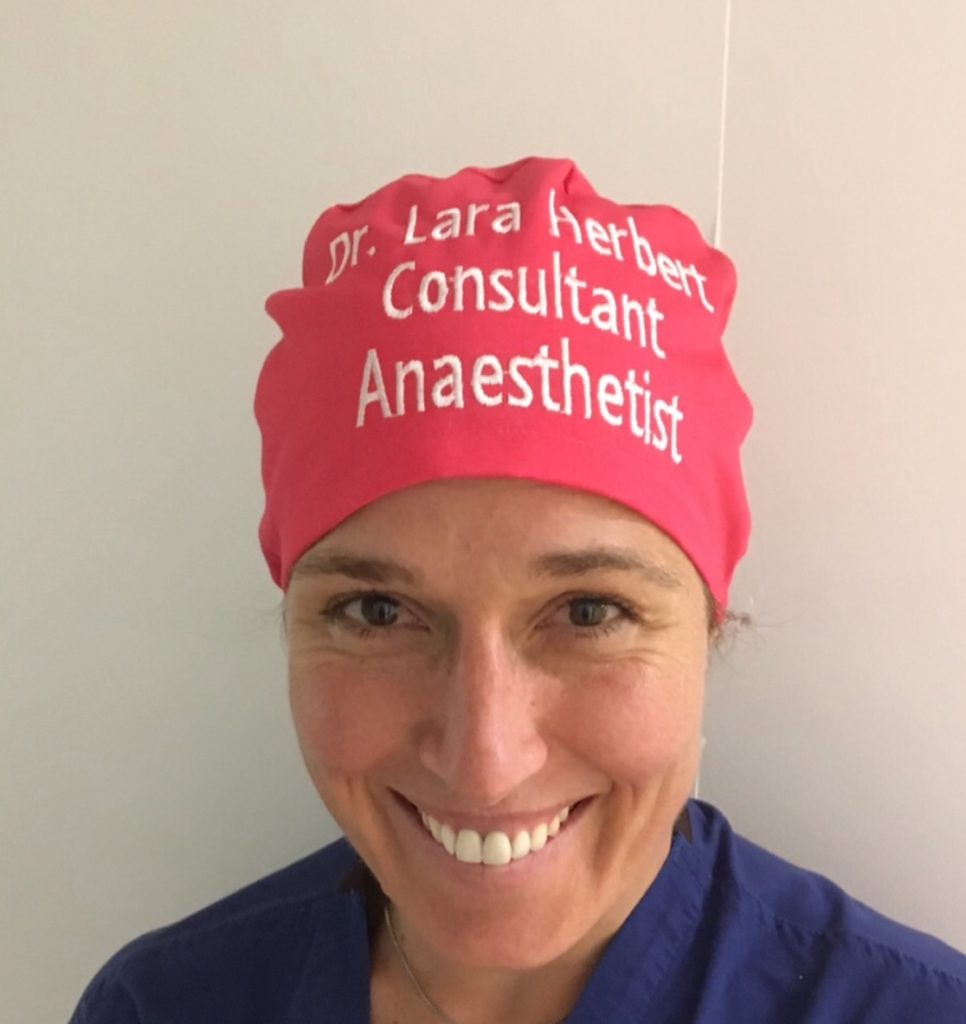
Where did you get that hat?
An increasing number of manufacturers supply name & role theatre hats. Please click on the images for link:
Please find a summary of extremely useful information for manufacturers – see here.
Please find a summary of extremely useful information for hospital trusts – see here.
Other options include stitched or iron on labels on hats. Below is a website offering such a service. There are many more on the internet:
For those healthcare staff who wouldn’t usually wear theatre caps as part of their standard uniform please do display your name and role in clear font. Show your support for the #hellomynameis campaign started by the late Kate Granger. Click on image below for web link:
What name should I choose to be addressed by?
There are certainly cultural differences which we need to understand when choosing the name by which we choose to be addressed.
Some will rightfully choose to be addressed by their surname with title – eg Dr Hackett
Some may like their full name with title eg Dr Robert Hackett – this may help staff with documentation when full names are required
Some may be concerned about using their real name at all concerned about security issues – of note London Transport allows staff to choose an alias if they are concerned about this – perhaps as long as one responds to the alias when it is used that is still beneficial (see here).
Some, particularly female doctors, have chosen to use their first name and title eg Dr Libby – to decrease their being confused with nursing staff created by sexual stereotypes.
In an extensive study ‘the vast majority of junior doctors consider the consultants they address informally to be more approachable’ (see here).
Thank you to everyone who supports this initiative. Thank you to those who continue to provide independent data on the impact of displaying names & roles.
A particular thank you to Dr Rhys Thomas, Alison Brindle and #hellomynameis Kate Granger & Chris Pointon.
We are doctors, nurses, midwifes, ODPs and other healthcare staff – we are dedicated and work as thoroughly as we can yet like all humans we will make mistakes. We can’t change this human condition but for patient safety we can change the conditions humans work within.

Name & Role theatre hats receive official endorsement from the Australian Society of Anaesthetists:
The #TheatreCapChallenge is supported by the American College of Anesthesiologists and the European Society of Anaesthesiology:
Name & Role theatre hats receive official endorsement from the American Association of Surgical Physicians Assistants:
The #TheatreCapChallenge supported by ANZCA via its bulletin:

#HelloMyNameIs #TheatreCapChallenge a please click on the image below to see Chris Pointon’s inspirational TED talk about the #HelloMyNameIs campaign:
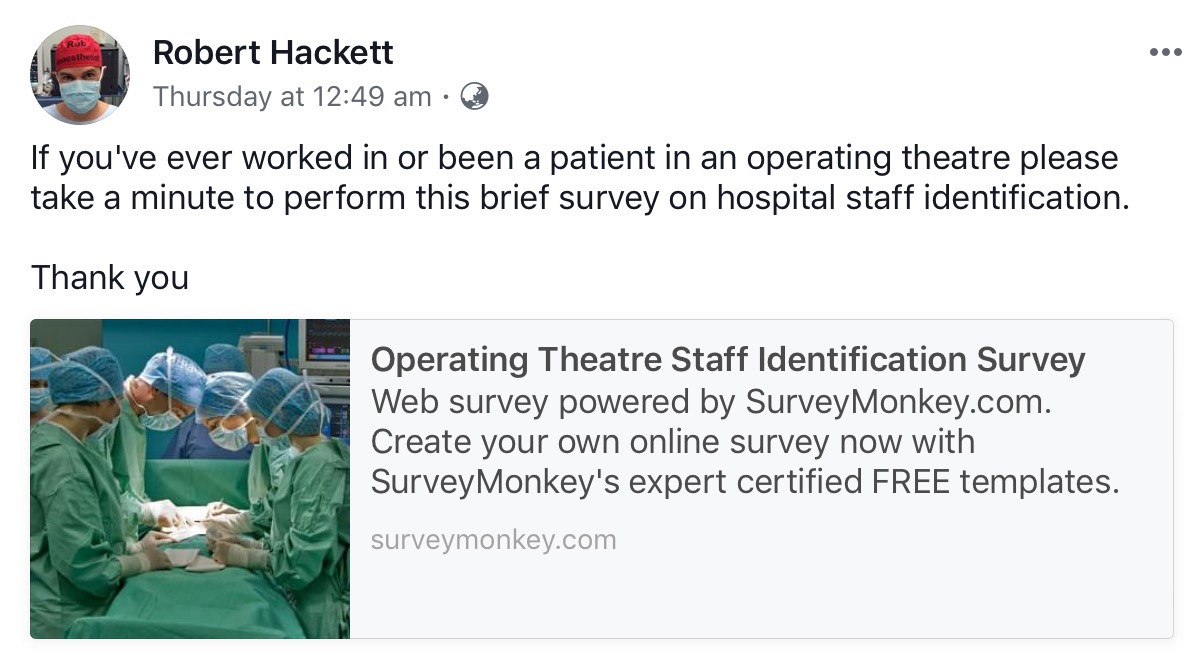
Please complete and share this very short (1 minute) survey looking at name and role identification (click on image below):
Please click on the image below, watch and share this brilliant #TheatreCapChallenge promotional video:
The #TheatreCapChallenge in mainstream media:
The #TheatreCapChallenge has been discussed in mainstream media internationally with write ups in Chinese, American, Russian, Japanese, Korean, Spanish and Indonesian newspapers.
Over 2 days it was the most read article in the Sydney Morning Herald with over 1 million reads on one day, over 300,000 likes and 30,000 comments which were strongly supportive. (see here).
#TheatreCapChallenge Hospitals